 For all the conversations happening about Ebola right now, startlingly few of them are practical. One question that all healthcare systems ought to be asking themselves right now is not only are they equipped to treat an Ebola patient, but can they afford it?
For all the conversations happening about Ebola right now, startlingly few of them are practical. One question that all healthcare systems ought to be asking themselves right now is not only are they equipped to treat an Ebola patient, but can they afford it?
The Truth About Ebola
After the first patient with Ebola in the U.S., Thomas Duncan, passed away Texas Health Presbyterian Hospital reportedly faced as much as a half a million dollars in healthcare expenses for his treatment. Since the stakes are so incredibly high with a confirmed Ebola diagnosis, it might seem insensitive to attempt to put a price tag on the treatment. As we’ve seen with the other Ebola patients in the U.S., Amber Vinson, Nina Pham and Craig Spencer, early intervention and aggressive treatment are the difference between life and death.
There were a lot of questions raised about the quality of Thomas Duncan’s care and whether or not his race and/or lack of insurance coverage played a part. While there is demonstrable socioeconomic disparity in healthcare coverage, it’s more than likely that these factors in conjunction with the hospital and nation’s relative inexperience and unpreparedness for such a fight, ultimately was the difference between life and death in the inaugural case.
But with a half-million dollar price tag, which was ultimately futile since the patient was lost and two staff members who cared for him weren’t properly protected and subsequently developed the virus, there are probably a lot of hospitals wondering how much they should sock away in their “Ebola fund” as the winter wears on.
The course of treatment for Ebola is fairly involved, though with the exception of an illusive vaccine, most hospitals already have what they need: the question is, do they have enough?
Earlier this year as a saline shortage ran through U.S. hospitals, there was a bit of doomsday prepping as hospitals began to hoard this vital fluid. To any patient who is losing a lot of bodily fluids, from blood loss, vomiting or diarrhea, intravenous saline is an important measure to combat dehydration. In an Ebola patient, who can be suffering from intractable vomiting and seemingly non-stop diarrhea at the height of the illness, proper hydration is essential to survival.
For Nina Pham, her successful treatment took a 13-day inpatient stay and reportedly $110,000. Early estimates have shown that treating an Ebola patient at a U.S. hospital can cost upwards of $8,500 per day. A large percentage of this cost comes from the need to utilize intensive care services and procedures like dialysis – as well as maintain proper security around the area. Throw in the costs of biocontainment and experimental treatments and you’re inching closer and closer to that $500,000 benchmark.
So, who’s paying? Will hospitals be able to be fully reimbursed by the insurers if patients are insured? And just how much will they be able to be reimbursed? In a healthcare system that routinely puts caps on how much they’ll reimburse physicians, you have to wonder what the cut-off will be for Ebola patients, especially when patient outcomes may not ultimately be reflective of care quality – surviving Ebola involves a lot of factors that a hospital can’t control. But will that be taken into consideration?
Luckily, with ICD-10, Ebola will have its own code for billing – one thing that may cause problems before this shift occurs is that Ebola is nested under a standard code for all viral hemorrhagic fevers.
There’s also the question of worker’s compensation – in the case of the nurses in Texas, since they voluntarily treated Thomas Duncan, knowing the risk, is the hospital liable to help cover their medical costs since they were infected on the job? Or, by seeking volunteers, did the hospital administration side-step any financial liability? Will similar policies begin cropping up in hospitals nationwide in response?
Like the development of Ebola in exposed individuals, the health of the healthcare system’s response to Ebola still remains to be seen. In the meantime, what can you do for clinical improvement in your organization?
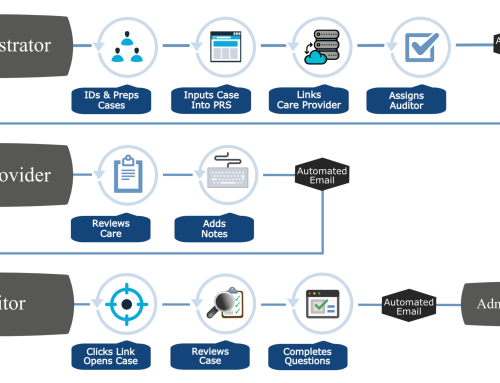
- If you haven’t already, set up screening tools and triggers in your EMR. Many have built-in checklists or warning screens to remind staff to ask about travel, exposure and any number of other customizable fields.
- Perform a strategic and organizational analysis – Analyze your organization’s past responses to smaller-scale outbreaks. Did you have a lot of Norovirus cases last year? Was there one year that sticks out in your mind as being an “unprecedented flu season”, or maybe a few years ago all the school kids got Hand, Foot and Mouth Disease. Look back at that data and ask yourself – what worked, what didn’t and start making changes right now.
- Train and retrain your staff and make sure that you communicate your expectations about reporting in the event of an Ebola case. Don’t leave any stones unturned. All staff, from housekeeping up to the C-Suite needs to know what to do, who to report to and how to protect themselves, the patient and other patients in the event of a confirmed (or even suspected case). Then, when you’ve laid out the plan – run a drill. Practice. Ask for feedback – and actually listen to it.
- Hold “town hall” meetings and invite staff, community and patients to share their concerns. This is not a time to cloister yourself in your office. Be clear, concise and confident. Don’t make promises you can’t keep but also don’t leave things so open-ended that all questions feel answered. Strive for a balance between informing and information-dumping.
- Reach out to others in your healthcare system, state and professional networks. Ask questions. Get ideas. Don’t assume that your plan is the best, that it’s foolproof or that it’s the only option you have. Sharing information and adapting good practices isn’t stealing – it’s learning.
- Identify local and regional health officials and have them on speed dial. Communicate your practices and procedures to them. Ask for advice if you aren’t sure if something is working. Ask them to keep you informed about updated policies and procedures as they are issued and reissued by the government. Keep your staff abreast of changes that affect their work.
- Make sure that your health information department as well as medical billers and coders all agree on how an Ebola case would be charted, abstracted and coded. Come to a consensus and stick to it. Ask your Clinical Documentation Improvement Specialists or nurses to help with this effort – and hold physicians accountable if their documentation is not up to par.



RT @BHMHealthcare: 7 Steps to Avoid Another Ebola – Like Pandemic http://t.co/eJVa7ERqbg