| BHM has solid experience and top level experts who understand the importance of the transition to value based reimbursement. Click here to find out more about how BHM can assist your organization. |
The healthcare industry is undergoing an inevitable shift away from fee for service payment models towards reimbursement models that align with the healthcare triple aim, such as value based payments. This significant departure from traditional models, which aligned reimbursement with care provided and rewarded by volume of care provided, focuses on performance and quality.
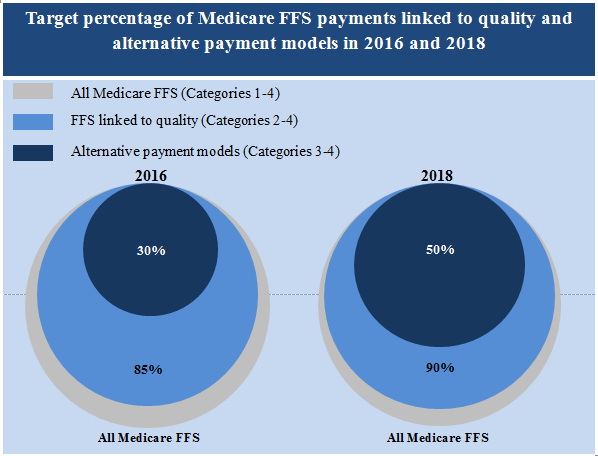
Now as part of healthcare reform, The Centers for Medicare and Medicaid Services (CMS) has allocated $10 billion dollars per year for the next 10 years toward reform initiatives which emphasize value based care.
The approach and question of which value-based model to implement still remains elusive for many organizations. Let’s take a look at some payment types on the value-based reimbursement spectrum.
Shared Savings
Low risk for providers with wide spread adoption. One of the least aggressive value based models.
- Paid as a fee for service model with bonuses provided if cost containment goals are met
- Incentive for achievement of quality goals
- No penalties for non-achievement of quality goals
Bundled Payments
Mid-level risk with moderate to widespread adoption, which is mandatory for some organizations/episodes of care.
- Flat rate payments are based on one episode of care (such as a specific surgery)
- Single flat rate payment applied to all providers involved with that episode across multiple care settings
Shared Risk
High risk with low adoption to date. One of the payment models expected to grow most rapidly in the coming years.
- Paid as a fee for service model
- End of year reconciliation of costs with performance bonuses provided for achievement of quality and cost containment goals
- “at risk” for spending which exceeds cost containment target
Capitation
This is the highest risk payment model and often used by Managed Care Organizations. Illness severity within specific patient populations can have dramatic bottom line impact if not monitored.
- Organizations receive a set payment amount per person per year with the expectation that high utilization population costs will be offset by low utilization population costs.
- If costs exceed allocation, the organization is “at risk” for covering the balance
- Requires complex cost containment, reporting strategies and population management capabilities
BHM has solid experience and top level experts who understand the importance of the transition to value based reimbursement. Click here to find out more about how BHM can assist your organization.