| The opioid epidemic is a real concern for health plans and providers. BHM understands the importance of how data management can be key to helping prevent opioid addiction. Click here to learn how we can help you. |
 The opioid epidemic sweeping the country is still in full force. As opioid dependency marks one of biggest challenges healthcare providers, payers, it has become a critical focus for everyone in the healthcare ecosystem. A recent study, reported by Kaiser Health News, found that the United States saw a 1300% spike in “spending by health insurers in a four-year period on patients with a diagnosis of opioid dependence or abuse.”
The opioid epidemic sweeping the country is still in full force. As opioid dependency marks one of biggest challenges healthcare providers, payers, it has become a critical focus for everyone in the healthcare ecosystem. A recent study, reported by Kaiser Health News, found that the United States saw a 1300% spike in “spending by health insurers in a four-year period on patients with a diagnosis of opioid dependence or abuse.”The study was conducted by FAIR Health, an organization dedicated to transparency in health care. In order to identify trends and pattern, the organization analyzed over 21 billion health claims. The health insurance companies they looked at represent over 150 million insured Americans with healthcare coverage.
The Opioid Epidemic Study Numbers
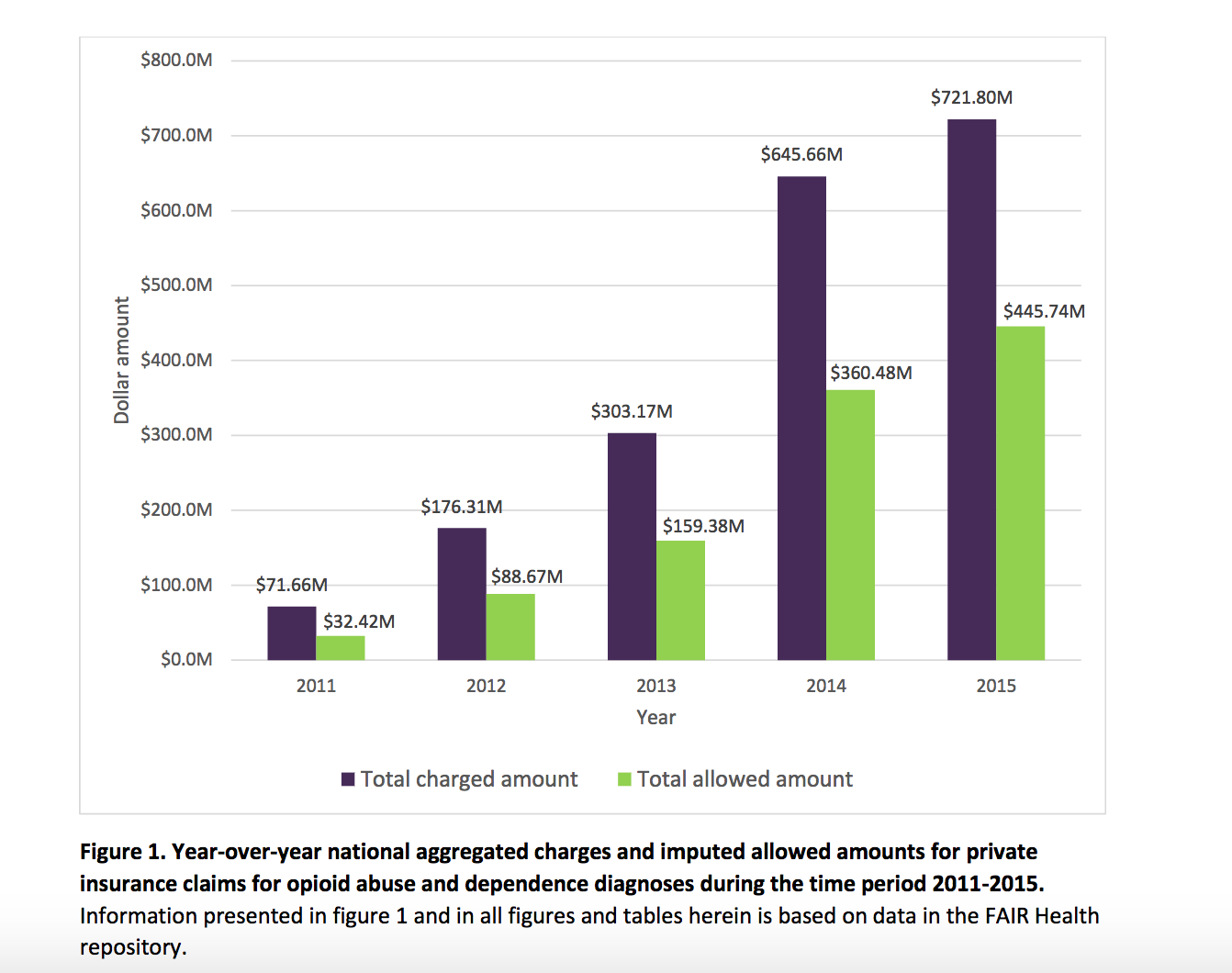
- 2011-2015: Payers’ payments to health systems and facilities reached $446 million, a 1375% increase from the previous $32 million.
- Insurers spend $19,333 on patients with an opioid dependence or abuse diagnosis. Compared to the $3,435 for an individual without a dependence diagnosis.
- There was 300% increase in the volume of claims connected with opioid dependence between 2007 and 2014.
- “Opioid abuse diagnoses involve significant emergency department charges , while opioid dependence charges are largely represented by laboratory tests and office outpatient visits²”
- “States’ average charges for services associated with opioid abuse and dependence diagnoses vary widely²”
- According to the claims the company studied, the highest set of services used were related to alcohol or drug therapy.
“Are medical school curricula adjusting to recognize the growing need for these services? Are insurers increasing the number of providers in their networks to ensure sufficient access? Are consumers being educated? It’s an issue that has to be dealt with in all quadrants¹.” Dr. Andrew Kolodny, senior scientist at Brandeis University
This study is a prime example of how much data gives insight for the future. When you analyze the effectiveness of prescription and pain management programs, you will learn what policies or processes need to be adapted and improved. Providers and payers should analyze data to effectively improve the way opioids are prescribed, used, and abused. This data is also crucial to patient safety and will help the opioid abuser get the help they need.
Sources
¹ Kaiser Health News: Study: Health Spending Related To Opioid Treatment Rose More Than 1,300 Percent
² FAIR Health Study – The Impact of the Opioid Crisis on the Healthcare System: A Study of Privately Billed Services