| CLICK HERE to speak with our Healthcare Experts and design the right plan for your organization. |
The Healthcare Effectiveness Data and Information Set (HEDIS) is used by more than 90 percent of health payers to assess and collect data on the performance of providers. HEDIS consists of a number of different measures on which healthcare providers are evaluated. Recent articles from healthpayerintelligence.com, identified the transition to value-based care as a significant factor for driving up HEDIS scores. Payers can hold providers accountable on how to quantifiably improve health outcomes.
Some major health insurance companies have gone forward with transitioning to value-based care payment platforms, which has required a greater focus on HEDIS quality measures.
For example, Humana released results showing that its value-based care model has boosted HEDIS quality scores by 19 percent when compared to its traditional fee-for-service Medicare Advantage plans.
“Our integrated approach to partnering with providers enables us to improve the health care experience for consumers in multiple ways,” said Bruce D. Broussard, Humana’s President and Chief Executive Officer.
The Humana value-based care platform also showed better patient outcomes:
- 6% decrease in emergency room visits
- 8% rise in the colorectal screening rate
- 13% increase in osteoporosis management
- 6% growth in breast cancer screening rates
Pain screening and medication review also saw an improvement of 5 and 6 percent.
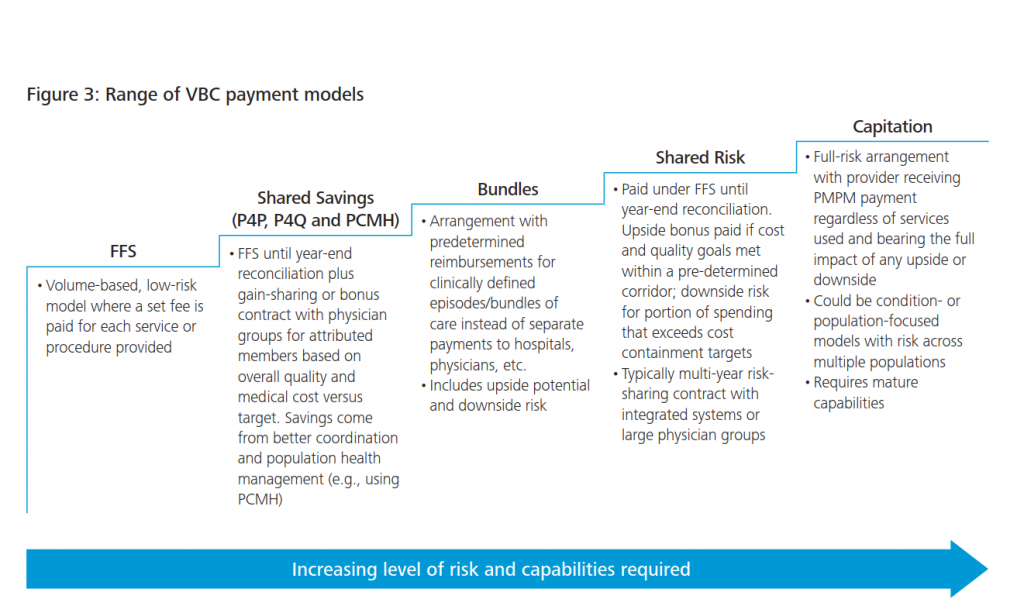
Figure comes from PwC report http://www.pwc.com/us/en/health-industries/health-research-institute/behind-the-numbers.html
Dr. Griffin Myers from Oak Street Health explained how his practice transitioned to value-based care under Humana’s leadership. “A value-based agreement drives our physicians to develop patient relationships where the goal is helping a patient reach his or her full health potential.”
The payer uses a pay-for-performance guideline that has reduced spending and improved clinical outcomes among its Medicare Advantage member population.
Check out other HEDIS articles from healthpayerintelligence.com