| Editor’s Note: Cost containment does not need to be a negative thing. Continual improvement strategies, by their nature, create efficiencies which lead to improved positive cost containment and management. Schedule a call with a BHM advisor CLICK HERE to learn more. |
B.E. Smith, an AMN Healthcare Company, released a 2017 Healthcare Trends Report recently. It collected a number of resources leading to a snapshot of overall healthcare spending. A summary of healthcare spending follows later in this blog and the full report is HERE. Positive Cost Containment
The takeaway from their data sources is, “All industry participants remain highly focused on containing costs.” Not a surprise, though 2017 may be a special year for sharpening pencils.
“You can’t cut your way to growth” – every successful executive
Where do we cut/go from here?
Managing resources, in 2017, suffers a negative brand image with many corporate cultures. Some organizations turned “managing resources” into a very positive experience.
Organizations with cultures of continuous improvement see increased cost control as a by-product of successful improvements. Starting with improvements and efficiencies as an ultimate goal sets a much more positive target than cutting, cutting, cutting.
Positive Cost Containment
Positive cost containment can begin with not paying for down time. Administrative resources dedicated to case and claim processing sit on your books as solid, steady expense while the processing pipeline swings dramatically. Paying overtime when backlogs occur will definitely impact the monthly administrative budgets. A number of other factors also contribute to these swings.
Retention and recruitment, in healthcare, can be a significant issue, and review services suffer two negative issues: behavioral health expertise and Chief Medical Officer turnover. “Some of the highest vacancy rates are for psychologists. National vacancy rate is 21% with a high of 64%.” – USA TODAY
Wouldn’t it be better if the human resources expenses devoted to maintaining consistency can focus on more positive projects? Image medical expertise devoted to patient care or system improvements?
Engaging a contractor specializing in physician advisor and peer-to-peer reviews can deliver unexpected benefits. One of BHM’s clients significantly increased their flow of reviews. When asked, they responded their on-time turnaround rate jumps around 40% with BHM reviewers. The quick ramping up of cases was because the comparative data proved a consistently better efficiency. Quicker TATs mean better control of workflow and expenses.
Cost containment does not need to be a negative thing. Continual improvement strategies, by their nature, create efficiencies which lead to positive cost containment and management. Schedule a call with a BHM advisor CLICK HERE to learn more.
Overall Healthcare Spending
Overall spending grew by grew slightly less (5.5% for the period October 2015 to 2016) than the estimate by CMS (5.8%) for all of 2015.1 Hospital care and nursing homes generated the largest increases (both over 6%). Prescription drugs claims jumped over 13% driven by an “increase in both the cost and use of specialty drugs.”2 Prescription drugs now account for 17% of employer health benefits.3 Figure here shows how U.S. healthcare spending is currently allocated.4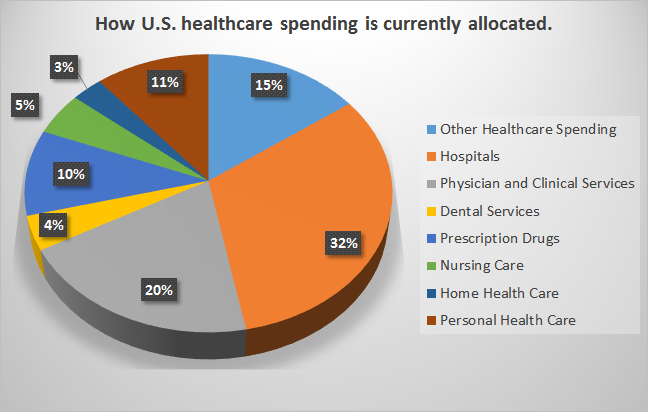
All industry participants remain highly focused on containing costs. While spending growth rates have been declining over the past decade, 2017 may reverse course. One leading forecaster predicts a 6.5% rise in 2017.5 This environment will prove challenging for providers. Moody’s believes “increasing supply costs and the possibility of wage pressure from the improving economy will add to margin pressure.”6 Fitch maintains a “stable” rating for non-profit hospitals for 2017, but a negative outlook with “slightly weaker” profitability and growing regulatory and political uncertainty. 7 That scenario could further strain a market characterized by 30% of hospitals running negative margins 8 and 8% of rural hospitals at “high risk of financial distress.” 9 Clearly healthcare organizations will not be able to relax their cost control diligence in 2017.
1 Altarum Institute, Spending Brief, “Insights from Monthly National Health Spending Data,” December 13, 2016.
2 D. Gowen, “Semi-annual carrier survey: Healthcare claim trend projections for 2017,” Wells Fargo Insurance Insights, May 2016.
3 Pricewaterhouse Coopers Health Research Institute, Medical Cost Trend: Behind the Numbers 2017, June 2016.
4 Altarum Institute, Spending Brief, “Insights from Monthly National Health Spending Data,” December 13, 2016.
5 Pricewaterhouse Coopers Health Research Institute, Medical Cost Trend: Behind the Numbers 2017, June 2016.
6 American Hospital Association. “2017 American Hospital Association Environmental Scan,” Hospitals & Health Networks, September 2016.
7 “Fitch Ratings Report: Not for Profit Outlook,” Business Wire, Dec 9, 2016.
8 American Hospital Association, “Trends in Hospital Financing,” TrendWatch Chartbook 2016.
9 North Carolina Rural Health Research Program, “Trends in Risk of Financial Distress among Rural Hospitals,” October 2016.