PwC’s Health Research Institute (HRI) released the results from a post-election survey focusing on models of health insurers of the future and the expectations of future members. The results and impacts outlined in their website report, identifies missions and investments for organizations best suited for targeted populations.
PwC’s Health Research Institute (HRI) released the results from a post-election survey focusing on models of health insurers of the future and the expectations of future members. The results and impacts outlined in their website report, identifies missions and investments for organizations best suited for targeted populations.
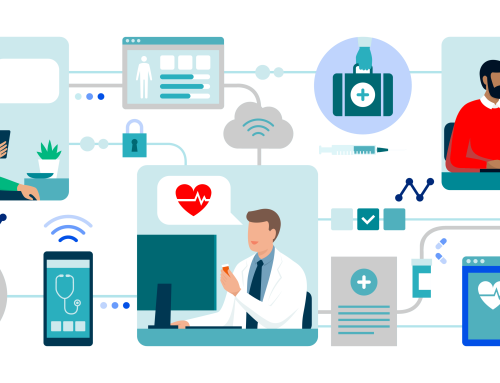
Models For Health Insurers Of The Future
Consumer Advocate: Empowers consumers through easy-to-understand, simplified plans and increased access to information. Often digitally enabled.
Bridge Connector: Facilitates the relationship between patients and care providers. Plays an active role in getting consumers the right care. Uses technology to enhance the provider and patient experience.
Analytic Sensor: Uses data analytics to give providers insight into the health of populations and provides solutions to help manage them. Pushes providers to value-based models to encourage keeping patients healthy.
Care Integrator: Integrates vertically to align incentives, improve care coordination, tackle utilization and keep medical costs low.
Lean Operator: Prioritizes gaining efficiencies with core health insurer functions (claims adjudication and payment, utilization review, etc.). May partner with company specializing in consumer engagement or provider enablement tools.
Why pursue Consumer Advocate model?
- Addresses the consumer’s increasing role in healthcare.
What health insurer today should consider these model in the future?
- Focus in the individual market.
- New entrants in the market (i.e. health insurance start ups).
- Strong technology capabilities.
- Locally or regionally focused.
What are potential investments to be made?
- Simplified plan design.
- Price transparency tools.
- Artificial intelligence technology.
- Self-service solutions and other consumer-facing technologies.
Which markets could be targeted?
- Tech-capable consumers to include healthy adults, seniors, and families.
Why pursue Bridge Connector model?
- Reduces medical costs for potentially expensive populations through increased communication between providers and patients.
- Meets providers’ demand for deeper connection with patients.
What type of health insurer should consider this model in the future?
- Focus on Medicare and Medicaid.
- Strong presence in communities with access to community resources and strong provider relationships.
- Locally or regionally focused.
What are potential investments to be made?
- Data analytics.
- Non-clinician health professionals.
- Retail storefronts to create consumer touchpoint.
- Telehealth to connect consumer and provider.
Which markets could be targeted?
- Consumers with complex chronic conditions or a desire for high-touch care, such as the frail elderly.
Why pursue Lean Operator model?
- Reduces costs by eliminating inefficiencies within core insurance and administrative functions.
What type of health insurer should consider this model in the future?
- Focus on providing administrative services to self-insured.
- Strong leadership to reach administrative targets.
- Broad geographical reach with large market share.
What are potential investments to be made?
- Blockchain to streamline claims processing.
- Identifying points of inefficiency.
- Partnering with companies that specialize in provider or consumer relations.
Which markets could be targeted?
- Self-insured employers looking to access core insurance functions and use other vendors to access additional services such as consumer engagement tools.
Why pursue Analytic Sensor model?
- Addresses demands for data analysis and increased focus on population health management.
- Provides opportunities for diversification into non-regulated lines of business.
What type of health insurer should consider this model in the future?
- Strong relationships with providers.
- Strong technology platform and analytics, or capital to invest in them.
- Broad geographical reach with large market share.
What are potential investments to be made?
- Data integration and analytics.
- Relationships with community resources.
Which markets could be targeted?
- Employers and providers looking to deploy population health strategies and individuals looking to reap benefits from leading a healthy life.
Why pursue Care Integrator model?
- Reduces medical costs due to lack of provider-payer alignment.
- Addresses providers’ interest in provider-sponsored health plans and vertical integration.
What type of health insurer should consider this model in the future?
- Robust financial reserves and revenue sources.
- Strong leadership
- Locally or regionally focused
- Densely populated market with strong market share or a provider with strong brand.
What are potential investments to be made?
- Acquisition of providers (hospitals, clinics, physicians) to integrate along care continuum.
- Data integration.
- Technology focused on enhancing continuity of care.
Which markets could be targeted?
- Consumers who highly value continuous care and convenience, to include healthy families as well as consumers with complex care needs.
About PwC’s Health Research Institute
PwC’s Health Research Institute (HRI) provides new intelligence, perspectives and analysis on trends affecting all health-related industries. The Health Research Institute helps executive decision-makers navigate change through primary research and collaborative exchange. Our views are shaped by a network of professionals with executive and day-to-day experience in the health industry. HRI research is independent and not sponsored by businesses, government or other institutions.