Proven Process for Payers To Maximize Efficiencies and Minimize Efforts
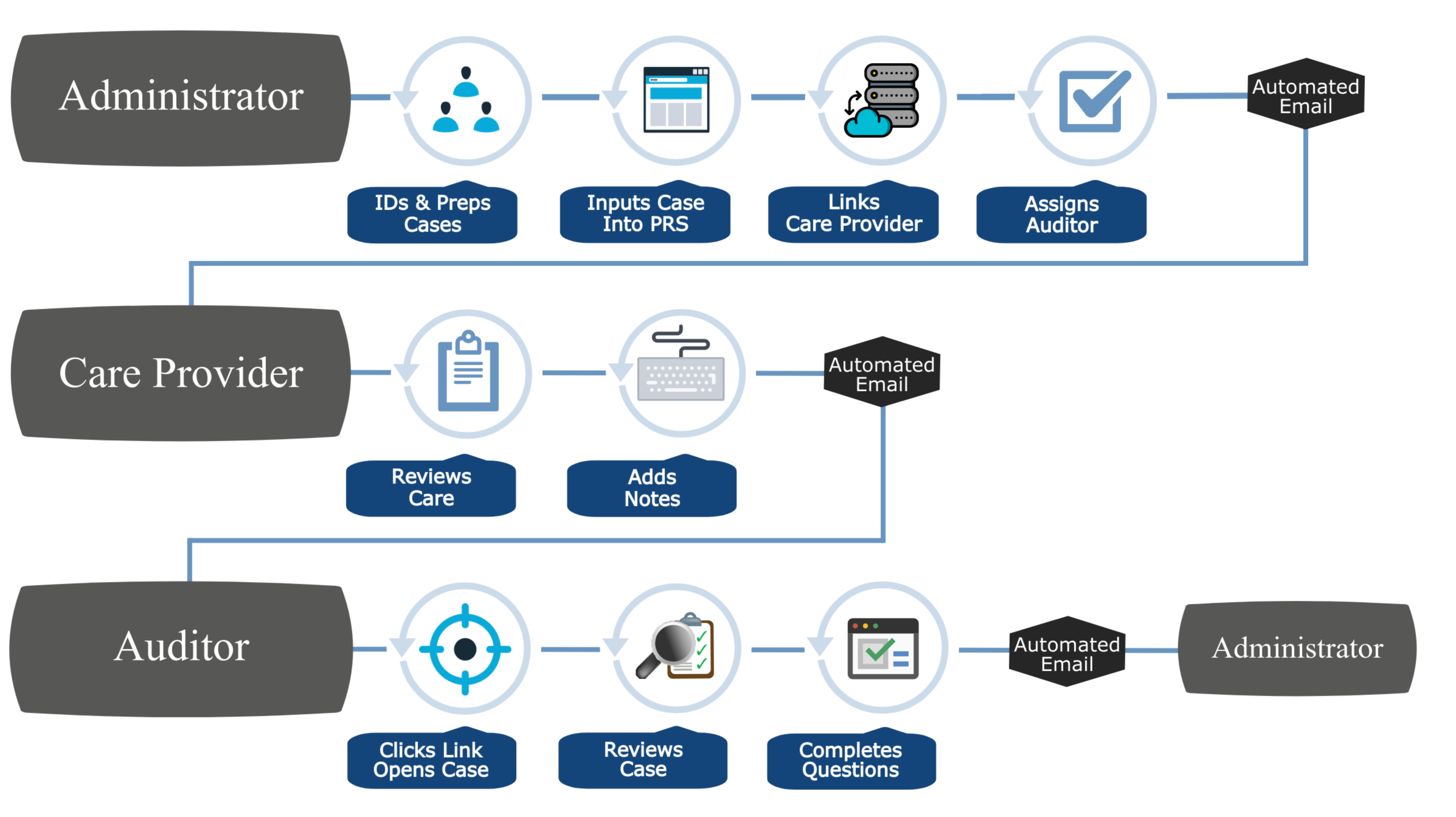
Elevate your payer operations with BHM's latest Insight. Unveil a proven process to maximize efficiency & minimize effort. Perfect your strategy and lead the way in healthcare management.