 Obamacare may impact healthcare quality improvement initiatives
Obamacare may impact healthcare quality improvement initiatives
Can quality be legislated? Perhaps so. The Heritage Foundation, a research and educational institution, states that “The Patient Protection and Affordable Care Act of 2010 (Obamacare)
So, you might reasonably ask, what is pay-for-performance? The Health Resources and Services Administration (HRSA), describes pay-for-performance as a system in which “providers are compensated by payers for meeting certain pre-established measures for quality and efficiency. Pay-for performance-programs have been implemented by both Medicare and private insurers. The Center for Medicare and Medicaid Services (CMS) has numerous demonstration projects underway to pilot these programs in a range of care settings, from primary care clinics to hospitals. Pay-for-performance can be seen as a means of attaching financial incentives to clinical care objectives. Using quantitative metrics, a percentage of physician compensation can be tied to achieving specific clinical benchmarks in the care they provide.”
How will “healthcare quality” be defined?
HRSA defines three dimensions of healthcare quality, which are:
- Structure, which represents the attributes of settings where care is delivered
- Process, or whether or not good medical practices are followed.
- Outcome, which is the impact of the care on health status.
In a report titled Crossing the Quality Chasm, The Institute of Medicine (IOM) identifies six essential characteristics of healthcare quality:
- Safe: avoiding injuries to patients from care that is intended to help them.
- Effective: providing services based on scientific knowledge to all who could benefit, and refraining from providing services to those unlikely to benefit (avoiding underuse and overuse).
- Patient-centered: providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide clinical decisions.
- Timely: reducing waits and sometimes harmful delays for both those who receive and give care.
- Efficient: avoiding waste, such as waste of equipment, supplies, ideas, and energy.
- Equitable: providing care that does not differ in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
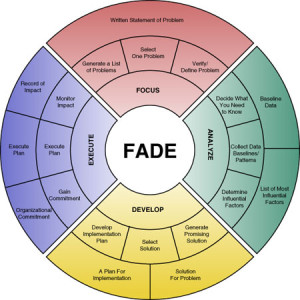
Now that we’ve established a fairly firm idea of what may constitute “healthcare quality” in this brave new world, we’ll need to establish a plan of action for improving it. Duke University has developed a QI (quality improvement) model that it refers to as FADE, an acronym for the following four steps:
- Focus: Define and verify the process to be improved.
- Analyze: Collect and analyze data to establish baselines, identify root causes, and point toward possible solutions.
- Develop: Based on collected data, develop action plans for improvement, including implementation, communication, and measuring/monitoring.
- Execute and Execute: Implement action plans, on a pilot basis, and install an ongoing measuring/monitoring (process control) system to ensure success.
HRSA explains that all successful quality improvement initiatives incorporate the following four key principles:
1. Consider both systems and processes.
To make improvements in healthcare quality, an organization needs to understand its own delivery system and key processes. Therefore, to improve quality of care (outputs/outcomes), the QI initiative must simultaneously consider both (inputs) and activities carried out (processes).
2. Focus on patients.
An important measure of healthcare quality is the extent to which patients’ needs and expectations are met. Services that are designed to meet the needs and expectations of patients and their community include:
- Systems that affect patient access
- Care provision that is evidence-based
- Patient safety
- Support for patient engagement
- Coordination of care with other parts of the larger health care system
- Cultural competence, including assessing health literacy of patients, patient-centered communication, and linguistically appropriate care
3. Focus on being part of the team.
A team approach is most effective when:
- The process or system is complex
- No one person in an organization knows all the dimensions of an issue
- The process involves more than one discipline or work area
- Solutions require creativity
- Staff commitment and buy-in are needed
4. Focus on use of the data.
Data is the cornerstone of QI and a key to boosting healthcare quality. It is used to describe how well current systems are working, what happens when changes are applied, and to document successful performance. Using data:
- Separates what is thought to be happening from what is really happening
- Establishes a baseline (Starting with low scores is ok)
- Reduces placement of ineffective solutions
- Allows monitoring of procedural changes to ensure that improvements are sustained
- Indicates whether changes lead to improvements
- Allows comparisons of performance across sites
Like to know more about quality improvement?
Quality improvement is a crucial element of your operations. BHM offers the expertise you need to achieve better outcomes at lower costs. Contact us today to find out how BHM’s proven strategies can work for you. Simply click below to get started







RT @BHMHealthcare: The Drive for Healthcare Quality and Pay for Performance: Obamacare may impact healthcare quality improvement… http://…
The Drive for Healthcare Quality and Pay for Performance http://t.co/UxuFKOhGwJ
#acaupdate…Duke studies prompt #ACA QI program…“Obamacare may impact healthcare quality improvement initiatives”… http://t.co/Ux8YOetXxS