 Summary: One of the latest healthcare buzzwords has been Population Health Management. The following article will discuss the correlation between Population Health Management and Readmissions.
Summary: One of the latest healthcare buzzwords has been Population Health Management. The following article will discuss the correlation between Population Health Management and Readmissions.
To say healthcare spending is out of control is putting it mildly. One of the high contributors to healthcare costs is the treatment of chronic conditions. In order to get a handle on these costs, the government has implemented a couple of initiatives: assessing penalties to hospitals with higher than average readmission rates and population management.
Readmission Penalties
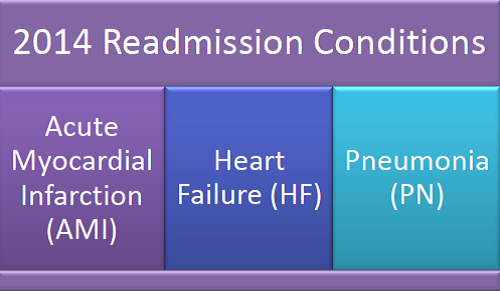
For 2014, hospitals will be assessed penalties for readmissions for Acute Myocardial Infarction, Heart Failure, and Pneumonia. The current readmission rate is 20%+. The penalty applicable began as up to 1% reduction in Medicare reimbursement with increases slated up to 3% as the program progresses. A readmission is defined as an inpatient admission within 30 days.
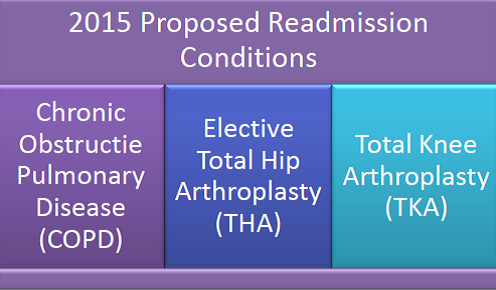
In 2015, CMS has proposed 3 additional conditions to be added to the readmission penalty program:
Population Health Management
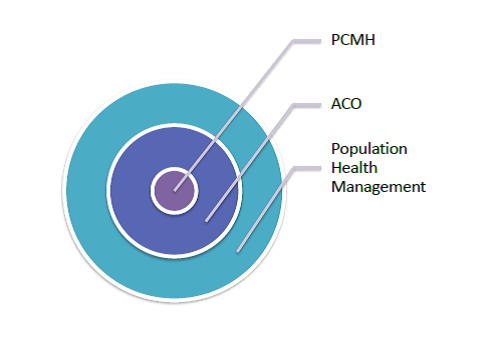
Population Health Management is built on the foundation of the Patient-Centered Medical Home (PCMH) and the medical home neighborhood, Accountable Care Organization (ACO). A PCMH is a healthcare model which places the individual/patient at the center of his/her care. The primary care physician is responsible for coordinating care with hospitals, home health agencies, mental health providers, as well as community organizations that encourage healthy living, wellness, and safe environments. ACOs are groups of PCMH’s working collaboratively to reduce costs and increase quality, while maintaining a patient-centered focus.
Population health management can be defined as the coordination of care across a population (either a total population or a population attributed to a particular chronic disease) to improve clinical and financial outcomes. To accomplish this, providers and organizations analyze patient data, identify gaps in care and deliver outreach. Gaps become even more prevalent as individuals are diagnosed with multiple chronic conditions.
The goal of Population Health Management is to provide patient-centered care focused on wellness as opposed to acute episodes of care. Responsible population management is the key to improving care quality and maximizing reimbursement while reducing costs. The aim is to be able to analyze populations, identify individual health risks, and deliver care as appropriate in the proper setting. The key to maintaining health and preventing illness is technology.
Population Health Management requires a shift in mindset from reactive to proactive, from treatment to prevention. The number of individuals eligible for chronic care treatment is increasing at a rapid rate due to the ACA. The ACA, as of 2014, extended coverage through offering health insurance exchanges as well as expanding Medicaid. Additionally, the population as a whole is aging. These factors make population health management almost critical. Population management focuses on the entire population of a practice with sub-populations that focus on specific chronic conditions, such as diabetes, asthma, congestive heart failure, hypertension, arthritis, sleep apnea, chronic obstructive pulmonary disease, and certain cancers. Do these sound familiar? They should. Some of these are the focus diseases targeted under the Affordable Care Act as they relate to readmissions and are listed above. Managing chronic conditions is one of the most important functions of population health, particularly when it comes to reducing costly hospital readmissions.
In summary, healthcare costs continue to rise. Chronic conditions continue to account for higher proportions of the cost. In order to try to reverse the trend, 2 intiatives have been put in place: assessing hospitals with readmission penalties if rates are too high and managing populations based upon specific chronic diseases through analysis, identifying care gaps, and putting protocols in place to address and treat these populations.





