| BHM understands the importance of the transition to value-based reimbursement. Clinical Case Shaping leverages our physician advisory network to identify gaps in meeting medical necessity criteria and addresses the entire case. Click here to learn more options and how BHM can improve your VBC efforts. |
Value-based care transition tough for providers. They are encountering significant challenges with limited access to claims data, risk-based insurance contracts, as well as investment capital.
The Centers for Medicare & Medicaid Services (CMS) has been pushing value based models that focus on quality of care rather than quantity. This means that most traditional incentive based payment models are being put phased out. The CMS hopes to tie 90% of all Medicare payments to alternative payment methods by 2018. Unlike fee-for-service models, value based models tie quality and cost together. By doing this they can encourage providers to give the best possible care at the best possible cost.
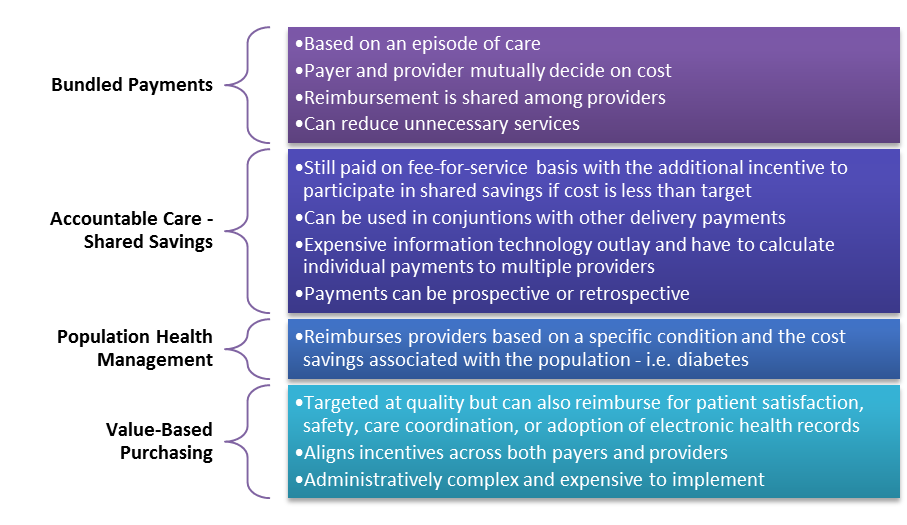
Many different levels exist for VBC:
These are the results in the Second Annual Member Survey by the American Medical Group Association (AMGA), which represents medical groups, health systems and other organized systems of care. The full results can be found here.
“Providers must be able to access administrative claims data in both the federal and commercial settings. Without a complete picture of a population of patients, it is virtually impossible to manage the cost and quality of a patient’s care. While some payers provide this data to clinicians, many do not.” – white paper detailing the results of AMGA’s survey
Among the obstacles to risk identified in the latest AMGA survey:
- Immature risk market: 64% report none to limited commercial value-based products locally.
- Lack of access to claims data: Providers are not able to access administrative claims data from all payers or encounter significant restrictions.
- Non-standard data: Providers report the massive administrative burden of submitting data in different formats to different payers.
- Limited access to capital Value-based care transition tough
- Inadequate infrastructure: Necessary systems—including information technology—is expensive and difficult to implement.
In a meeting to the incoming administration AMGA recommends the following to reduce the hurdles standing in the way of providers:
- Congress should require federal and commercial insurance companies and providers to standardize data submission and reporting processes
- Congress should create a fund that enables providers to use income on a tax-free basis for reinvestments
- Congress should not penalize Advanced APMs if there are insufficient risk products in their local markets
BHM understands the importance of the transition to value-based reimbursement. Clinical Case Shaping leverages our physician advisory network to identify gaps in meeting medical necessity criteria and addresses the entire case. Click here to learn more options and how BHM can improve your VBC efforts
Summary data collected by Greg Slabodkin, published December 09 2016, by healthdatamanagement.com. Health Data Management is the information resource for medical and IT professionals, executives and administrators who are leading the transformation now sweeping the healthcare industry. Value-based care transition tough