 Summary: The key to increased revenue in the Emergency Room is a patient-centered focus.
Summary: The key to increased revenue in the Emergency Room is a patient-centered focus.
Patient-Centered Focus Patient Perspective
As a patient, one of the main healthcare criticisms is waiting for hours and hours in the Emergency Department (ED). Many times we lose sight of the patient’s perspective. Patients in the ED, in their minds, need to be seen immediately or they might have gone elsewhere for treatment such as urgent care clinics or their primary care physician. The ED is generally a place of last resort, when there is nowhere else to turn. These patients are generally in pain and or suffering from acute illnesses. As much as we are concerned with “herding patients in and out of the ED”, you have to stop and put yourself in the patient’s shoes. That being said, EDs are notorious for extended wait times (lengths of stay), which increases the general agitation level of these patients. ED patients want to be seen, be treated quickly, and released as quickly as possible in order to return home and begin to recuperate.
Patient-Centered Focus ED Perspective
From an ED perspective, EDs are a natural bottleneck. EDs are generally chaotic to put it mildly. There is always a flurry of activity from patients flooding the entrances, to tired employees scrambling to keep up with the pace, to patient’s who code for heart or respiratory issues and need immediate attention, to psych patients who can be of danger to themselves and/or others. There is no rest for the weary. There is little to no downtime. The atmosphere in and of itself lends itself to high anxiety among caregivers and support staff.
Patient-Centered Focus – Reducing ED Wait Times
So, we have high anxiety levels from both the patient and caregiver perspective. What can be done to make the experience, I won’t say enjoyable, but tolerable, given the circumstances? How do we reduce ED wait times, work more efficiently, and most importantly, provide excellent and timely patient care? One answer, although small in the grand scheme of things is to start from the beginning of the patient experience – when the patient walks in the door. How does the triage process work? Are there processes/protocols in place to determine whether a patient is likely to be treated and discharged within the same day, whether the patient will likely require additional treatment and may stay up to 48 hours, or whether the patient will likely be admitted and require a 3-7 day inpatient stay?
The Emergency Department triage process is critical to reducing ED wait times, maximizing reimbursement, improving customer satisfaction and most importantly providing excellent patient care. Long wait time and inefficiencies in the throughput process add substantially to the already high costs of healthcare. Customer satisfaction is one of the keys to reimbursement. Long wait times in the ED can negatively affect patient satisfaction and consequently reduce reimbursement. Many hospitals are so focused on the bottom line that they forget why they are in business – to provide excellent patient care. So, it would seem, if the emphasis is shifted from healthcare costs to quality patient care, the profitability will naturally follow. So, let’s make the ED visit as painless as possible for the patient. Put yourself in the patient’s shoes.
Patient-Centered Focus – 2 Midnight Rule
CMS has issued guidelines to improve ED throughput and enable patients to be treated in the most appropriate settings to ensure the quality of care and safety of the patient remain the focus. In fact, following these guidelines is a win-win for both the patient and the ED. In August 2013, CMS released a new rule, CMS-1599, which is commonly referred to as the “2-Midnight Rule”. The 2-Midnight Rule is provides reimbursement for “observation patients”, those who are slated to be treated within the hospital and released between 8 hours and “2 midnights”. This category of patients are generally placed in ED pods in a separate section of the ED, out of the general waiting room. Patients are evaluated and treated within the confines of these pods. It is basically an intermediate level of care – between treatment/discharge and inpatient admission. The 2-Midnight Rule provides reimbursement for patients properly categorized who need additional observation beyond the standard ED visit but who will be discharged within 2 midnights.
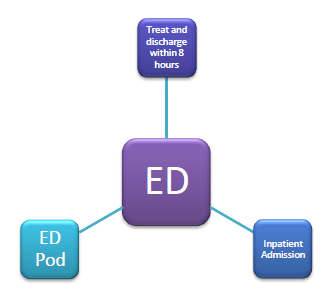
There are 3 groups of ED patients:
- Category 1 – those who will more than likely be treated and released in less than 8 hours
- Category 2 – those who will more than likely be treated and released between 8 hours and 2 midnights
- Category 3 – those who will more than likely be admitted and remain as inpatient for greater than 2 midnights.
Establishing protocols to properly categorize ED patients based upon medical necessity criteria will increase throughput in the ED and enable patients to be treated more efficiently and more effectively. Patients who are due to be discharged within 8 hours should be assessed, treated, and discharged as quickly as possible. Those that will require additional observation should be assigned to ED pods where treatment can be administered. Those that will require additional treatment beyond observation should be evaluated as soon as possible and moved to the inpatient setting. Following these 3 triage categories will reduce ED wait times, increase patient satisfaction, and drive revenue.
A lot of revenue is lost through not designating and treating patients appropriately in terms of length of stay. If the stay in the ED is longer than 8 hours, you may not receive full reimbursement. If admitted but patient only stays for 2 days, you may not receive full reimbursement. If observation pods/days aren’t utilized appropriately, you may not receive full reimbursement. Are you leaving revenue on the table? Do you need assistance with reducing ED wait times, increasing patient satisfaction, and improving ED throughput?
About BHM – https://bhmpc.com/
BHM Healthcare Solutions is a healthcare consulting firm which has assisted many clients in recouping revenue and increasing their bottom line. Contact us to see how we can best assist you from developing protocols to training to assessing. 1=888-831-1171 or re*****@*******pc.com.
Click below to request additional information to find out how BHM can best be of assistance to you.

