| . CLICK HERE to learn more about how BHM helps your organization. |
New research shows that accountable care organizations are partnering with community resources and social service agencies to improve population health management according to a new report from Premier Inc., Performance Evaluation: What Is Working In Accountable Care Organizations? Highlights from the study are presented here.
Private payers and the alternative payment models they’ve used among accountable care organizations have shown mixed results, but coordinating with social service agencies may bring improvements in population health management. Coordination with community centers will take the hospital-centered approach to healthcare in a significantly different direction, the report states [email-download download_id=”69912″ contact_form_id=”67945″]
As one of the main purposes of ACOs is to reduce cost through improved care coordination and optimizing care provision, several respondents pointed to categorizing patients based on risk factors and then targeting them for specific interventions. Others mentioned reducing readmissions through better coordination with physician practices and moving to generic or less expensive alternative medications.
Example clinician response
The second area that we became a little bit concerned about was the number of rising risk patients…So we did some benchmarking, and we’ve adopted a model that is called coaching. So these are actually kind of high end MAs, medical assistants, that are working along with our primary care physicians and our care managers to look at patients who are in that rising risk category who maybe have some social issues, some compliance issues, maybe some educational issues, and these coaches are actually spending a lot of time working with those patients, whereas the primary care physician probably would not have time. The full reason for that is to really prevent them from moving up into the high risk category. So we have had some good results from that program as well.
The full 85 page report includes testimonies from the survey from respondents.
In an article by Vera Gruessner on xpanding their reach toward community service organizations and the patient community is expected to help accountable care organizations improve their population health management strategies.
ACOs are not paid to provide transportation, offer health fairs, perform home modifications, etc. However, despite the lack of funding and history of supporting this work, some ACOs are stepping up and expanding their services beyond traditional clinical services and to more than just their assigned beneficiaries.
The researchers found that ACOs have been working to provide transportation and modify patients’ homes to ensure their well-being. Some accountable care organizations have become the central arena where community service agencies have functioned through to reach patients in need of mental health assistance or drug dependency rehabilitation.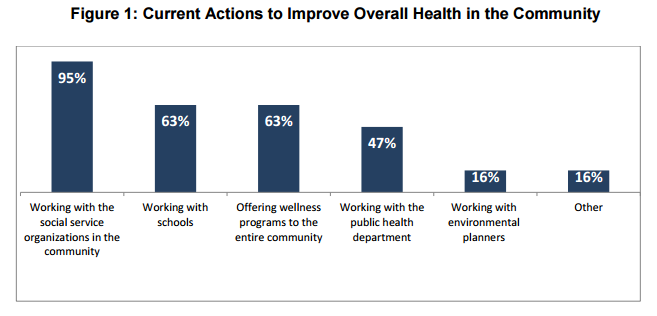
When providers and accountable care organizations embrace the use of population health management and value-based care reimbursement, the quality of patient care can be improved while overall healthcare spending is likely to decrease. For example, one ACO, the Great Lakes Organized System of Care, has been able to reduce the rate of hospital readmissions and increase the number of cancer screenings through greater patient outreach.
BHM Healthcare Solutions, Inc., works with both payers and providers for integrated solutions to the challenges of modern healthcare.
BHM, Behavioral Health and Medical Review Experts, providing behavioral health and medical review services and performance improvement consulting to health plans, providers, ACOs, TPAs, workers’ compensation and other insurers nationally. With our services, BHM emphasizes value, quality, and affordable pricing. BHM assists clients reacting to healthcare regulation problems and those wanting to proactively improve operational efficiencies.

