 Levels of Care Guidelines are usually derived from generally accepted standards of behavioral health practice. These standards include guidelines and consensus statements produced by professional specialty societies, as well as guidance from governmental sources such as CMS’ National Coverage Determinations (NCDs) and Local Coverage Determinations (LCDs). Level of Care Guidelines are also developed from input provided by clinical personnel, providers, professional specialty societies, consumers, and regulators.
Levels of Care Guidelines are usually derived from generally accepted standards of behavioral health practice. These standards include guidelines and consensus statements produced by professional specialty societies, as well as guidance from governmental sources such as CMS’ National Coverage Determinations (NCDs) and Local Coverage Determinations (LCDs). Level of Care Guidelines are also developed from input provided by clinical personnel, providers, professional specialty societies, consumers, and regulators.
Medical necessity is a medical claims determination which encompasses outcomes which are justified as reasonable, necessary, and/or appropriate based on evidence-based clinical standards of care. Evidence-based medicine (EBM) aims to apply the best available evidence to clinical decision making. It seeks to assess both the of risks and benefits of treatments and diagnostic tests and assists clinicians in determining whether or not a treatment will do more harm than good. [email-download download_id=”7229″ contact_form_id=”68021″]
From the CMS website, Medical review (clinical review) is the collection of information and clinical review of medical records by Medicare Contractors to ensure that payment is made only for services that meet all Medicare coverage, coding, and medical necessity requirements. Medical review activities are directed toward areas where data analysis, Comprehensive Error Rate Testing (CERT) and Office of Inspector General (OIG)/Government Accounting Office (GAO) findings as well as Recovery Audit Contractor (RAC) vulnerabilities indicate questionable billing patterns.
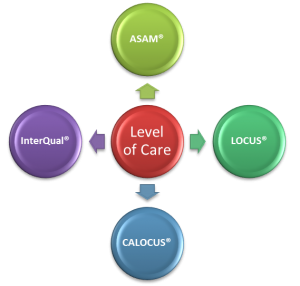
Levels of Care
Levels of care classify health care into categories of chronology, priority, or intensity, as follows:
- Emergency care handles medical emergencies and is a first point of contact or intake for less serious problems, which can be referred to other levels of care as appropriate.
- Intensive care, also called critical care, is care for extremely ill or injured patients. It thus requires high resource intensity, knowledge, and skill, as well as quick decision making.
- Ambulatory care is care provided on an outpatient basis. Typically patients can walk into and out of the clinic under their own power (hence “ambulatory”), usually on the same day.
- Home care is care at home, including care from providers (such as physicians, nurses, and home health aides) making house calls, care from caregivers such as family members, and patient self-care.
- Primary care is meant to be the main kind of care in general, and ideally a medical home that unifies care across referred providers.
- Secondary care is care provided by medical specialists and other health professionals who generally do not have first contact with patients, for example, cardiologists, urologists and dermatologists. A patient reaches secondary care as a next step from primary care, typically by provider referral although sometimes by patient self-initiative.
- Tertiary care is specialized consultative care, usually for inpatients and on referral from a primary or secondary health professional, in a facility that has personnel and facilities for advanced medical investigation and treatment, such as a tertiary referral hospital.
- Follow-up care is additional care during or after convalescence. Aftercare is generally synonymous with follow-up care.
- End-of-life care is care near the end of one’s life. It often includes the following:
- Palliative care is supportive care, most especially (but not necessarily) near the end of life.
- Hospice care is palliative care very near the end of life when cure is very unlikely. Its main goal is comfort, both physical and mental.
Goal of the Physician Advisor Medical Review Program
The goal of the physician advisor medical review program is to reduce payment error by identifying and addressing billing errors concerning coverage and coding made by providers. To achieve the goal of the medical review program, Medicare Contractors:
- Proactively identify patterns of potential billing errors concerning Medicare coverage and coding made by providers through data analysis and evaluation of other information (e.g. complaints);
- Review CERT data, RAC vulnerabilities and OIG/GAO reports;
- Take action to prevent and/or address the identified error;
- Publish local medical review policy (called Local Coverage Determination-(LCD)) to provide guidance to the public and medical community about when items and services will be eligible for payment under the Medicare statute; and
- Publish MLN (Medicare Learning Network) educational articles as they relate to the medical review process.
Using Medical Necessity Criteria (MNC) successfully requires constant attention, understanding, and on-going education. BHM’s reviewer network MNC expertise allows you to focus on patient care. Click HERE and discuss how BHM’s MNC expertise can overcome medical necessity criteria challenges and improve your metrics.





