|
Payers are tasked with making complex coverage decisions that have far-reaching implications for patients, providers, and the healthcare system as a whole. From managing costs to ensuring quality care, these decisions require a deep understanding of the healthcare landscape, as well as strategic approaches to optimize outcomes. In this blog, we will delve into the key considerations for payers when navigating complex coverage decisions and how they can leverage expertise to achieve optimal results.
Understanding the Landscape
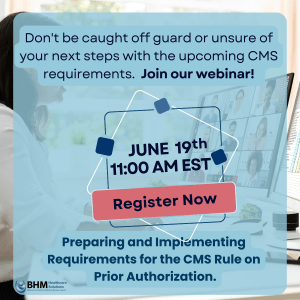
Click to register for our upcoming webinar on implementing the CMS Final Rule.
At the core of effective coverage decisions lies a comprehensive understanding of the healthcare landscape. Payers must stay abreast of the latest regulations, policies, and market trends that impact coverage decisions. This knowledge serves as the foundation for making informed decisions that are both compliant with regulatory requirements and responsive to market demands.
Utilizing Data Analytics
Data analytics is a powerful tool that can help payers make informed coverage decisions. By analyzing data on healthcare utilization, costs, and outcomes, payers can identify trends and patterns that can inform coverage policies. For example, data analytics can help payers identify high-cost areas where interventions may be needed to improve outcomes and reduce costs. Additionally, data analytics can help payers track the impact of coverage decisions over time, allowing for continuous improvement and optimization of coverage policies.
Engaging Stakeholders
Collaboration with stakeholders is essential for making coverage decisions that are effective and responsive to the needs of patients and providers. Stakeholders, including providers, patients, and policymakers, can provide valuable insights and perspectives that can help inform coverage decisions. For example, providers can offer insights into the clinical efficacy of treatments, while patients can provide insights into their preferences and needs. By engaging stakeholders in the decision-making process, payers can ensure that coverage decisions are well-informed and reflective of the needs of the healthcare community.
Leveraging Clinical Expertise
Clinical expertise is invaluable when making coverage decisions, particularly for complex medical conditions or treatments. Clinical experts can provide insights into the efficacy and safety of treatments, as well as their potential impact on patient outcomes. By leveraging clinical expertise, payers can make decisions that prioritize patient safety and quality of care.
Implementing Evidence-Based Medicine
Evidence-based medicine should form the foundation of coverage decisions. By relying on scientific evidence and clinical guidelines, payers can ensure that coverage decisions are based on the best available evidence. This can help payers avoid coverage decisions that are not supported by evidence and may not be in the best interest of patients.
Considering Patient Preferences
Patient preferences should also be considered when making coverage decisions. Understanding patient preferences can help payers design coverage policies that are patient-centered and responsive to patient needs. For example, some patients may prefer less invasive treatments, while others may prioritize treatment effectiveness. By considering patient preferences, payers can ensure that coverage decisions are aligned with patient needs and preferences.
Monitoring and Evaluation
Continuous monitoring and evaluation of coverage decisions are essential to ensure that they are effective and aligned with the goals of the payer organization. By monitoring outcomes and evaluating the impact of coverage decisions, payers can identify areas for improvement and make adjustments as needed. This can help payers optimize coverage policies over time and ensure that they are achieving the desired outcomes.
Adapting to Change
The healthcare landscape is constantly evolving, and payers must be adaptable in their approach to coverage decisions. Payers should be prepared to adjust their coverage policies in response to new evidence, market trends, and regulatory changes. By being proactive and adaptive, payers can ensure that their coverage decisions remain relevant and effective in a rapidly changing healthcare environment.