
Industry Watch Alert
The recent ARPA-H announcement outlining the ADVOCATE initiative signals a medium-to-high strategic impact for payers over the next 3–7 years.
While still research-stage, the concept of continuous, agentic AI–driven heart failure management points toward future pressure on utilization strategy, benefit design, and AI governance standards.
If validated, these models could materially reduce acute events in one of the highest-cost disease categories, while also accelerating expectations for transparency, auditability, and oversight across both clinical and payer-operated AI systems.
For payer leadership, the announcement functions less as a product launch and more as an early indicator of where regulatory, clinical, and public scrutiny around AI-enabled care delivery is heading.
Summary
 ARPA-H launched the ADVOCATE program to fund development of an FDA-authorized agentic clinical AI system designed to provide continuous, 24/7 cardiovascular care, beginning with heart failure. The initiative focuses on AI that can autonomously support care navigation, medication management, and clinical decision-making by integrating with EHRs, wearables, and existing clinical workflows, while remaining clinician-supervised.
ARPA-H launched the ADVOCATE program to fund development of an FDA-authorized agentic clinical AI system designed to provide continuous, 24/7 cardiovascular care, beginning with heart failure. The initiative focuses on AI that can autonomously support care navigation, medication management, and clinical decision-making by integrating with EHRs, wearables, and existing clinical workflows, while remaining clinician-supervised.
A defining feature of ADVOCATE is its emphasis on governance: the program includes development of a supervisory AI layer to monitor safety, performance, and bias of continuously learning clinical AI systems. If successful, ADVOCATE could shape future expectations for how autonomous clinical AI is deployed, regulated, and overseen across high-cost chronic disease management.
Executive Impact Analysis
Strategic Impact Assessment for Payers
This announcement signals a medium-to-high potential strategic impact on the healthcare payer landscape over the next 3–7 years, particularly in cardiovascular disease management, utilization control, and expectations around AI governance.
While the ADVOCATE initiative remains research-stage, its scope and design provide a credible preview of how agentic clinical AI could reshape payer decision-making frameworks if clinical and economic outcomes are validated.
Near-Term Payer Implications (1–3 Years)
Utilization patterns and cost management
If ADVOCATE demonstrates that continuous, AI-guided heart failure management can materially reduce hospitalizations and readmissions, payers will face increasing pressure to recognize and evaluate AI-mediated care models as legitimate cost-containment tools rather than experimental adjuncts.
Early implications are likely to surface first in pilot programs, value-based arrangements, and disease management carve-outs rather than broad benefit adoption.
Network and contracting considerations
Health plans may begin differentiating provider and vendor partners based on readiness to participate in AI-enabled cardiovascular management models. Over time, agentic AI capabilities could become a competitive factor in value-based and downside-risk contracts for high-cost CVD populations.
Medium-Term Implications for Coverage and Policy
Benefit design and coverage classification
An FDA-authorized “clinician-extender” capable of autonomous medication titration, guideline-directed medical therapy adjustments, and longitudinal care navigation challenges existing benefit categories. Traditional distinctions between telehealth, remote monitoring, DME, and software-enabled services may no longer be sufficient.
Payers should anticipate the need for new coverage definitions or policy clarifications as these models mature.
Prior authorization and medical policy evolution
As evidence accumulates that continuous AI-guided management prevents decompensation, payer medical policies may need to recognize AI-generated adherence, risk stratification, and longitudinal monitoring data as acceptable clinical documentation. This would represent a material shift in how clinical necessity is substantiated.
Risk Management, Oversight, and AI Governance
Rising expectations for model governance
ADVOCATE’s emphasis on a supervisory agent designed to monitor continuously learning clinical AI reflects emerging norms for transparency, bias detection, and auditability. Payers deploying AI across utilization management, claims editing, or risk adjustment should expect increased scrutiny of whether their governance frameworks meet comparable standards.
Regulatory and reputational alignment
Because the supervisory model is positioned as disease-agnostic and potentially open source, regulators and advocacy groups may increasingly reference it as a benchmark. This is especially relevant in the context of ongoing scrutiny around algorithmic decision-making in coverage determinations.
Implications for Value-Based Care Strategy
Expanded levers in cardiovascular value-based care
Agentic AI aligns naturally with shared savings, bundled payments, and capitated models for heart failure, one of the highest-cost chronic conditions. If validated, these tools could materially improve a plan’s ability to manage readmissions and total cost targets without expanding provider headcount.
Data integration and interoperability readiness
To capture value, payers will need analytics and interoperability capabilities that can ingest AI-generated insights from EHRs and wearables into care management, quality measurement, and population health programs. Without this infrastructure, potential savings may remain theoretical.
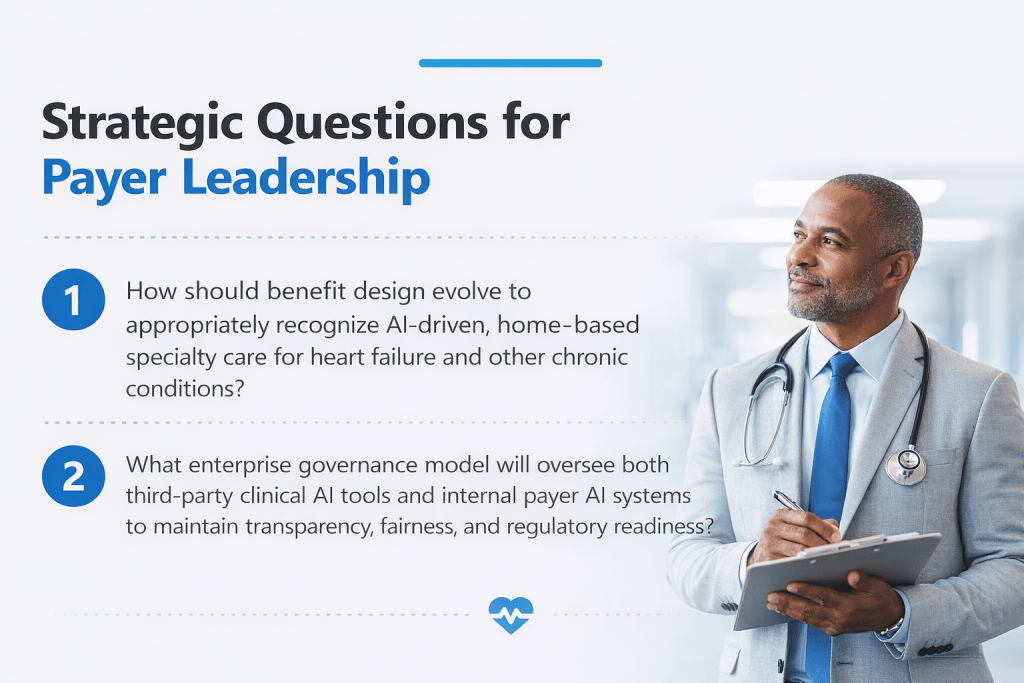
As agentic clinical AI moves closer to real-world deployment, payer organizations will increasingly be asked not just whether AI improves outcomes, but whether it is governed responsibly, integrated coherently, and aligned with coverage policy and regulatory expectations.
Navigating that shift requires:
Clear clinical oversight frameworks for AI-informed care
Medical policy structures that can adapt to non-traditional evidence sources
Governance models that apply consistently across third-party and internal AI systems
Organizations that address these questions proactively will be better positioned to evaluate innovation without increasing regulatory or reputational risk.
Clinical oversight grounded in both technological fluency and real-world utilization management experience becomes the differentiator as technology integrations accelerate. As a preferred vendor, BHM Healthcare Solutions brings decades of UM expertise, helping organizations apply innovation responsibly while maintaining rigorous clinical integrity.
Previous Alerts
Source
Each week, we email a summary along with links to our newest articles and resources. From time to time, we also send urgent news updates with important, time-sensitive details.
Please fill out the form to subscribe.
Note: We do not share our email subscriber information and you can unsubscribe at any time.
|
|
Thank you for Signing Up |

Partner with BHM Healthcare Solutions
BHM Healthcare Solutions offers expert consulting services to guide your organization through price transparency & other regulatory complexities for optimal operational efficiency. We leverage over 20 years of experience helping payers navigate evolving prior authorization requirements with efficiency, accuracy, and transparency.
Our proven processes reduce administrative errors, accelerate turnaround times, and strengthen provider relationships, while advanced reporting and analytics support compliance readiness and audit preparation. From operational improvements to strategic positioning, we partner with organizations to turn regulatory change into an opportunity for clinical and business excellence.
