
Industry Watch Alert
The Consolidated Appropriations Act, 2026 establishes near-term stability across several high-impact healthcare policy areas while extending pandemic-era flexibilities that materially affect payer operations. Most notably, the law extends Medicare telehealth authorities through 2027, preserves hospital-at-home programs through 2030, and delays Medicaid DSH payment reductions until 2028.
For payer organizations, the legislation reduces immediate disruption but reinforces longer-term governance challenges tied to telehealth utilization, alternative site-of-care models, and Medicaid financing. The Act does not introduce sweeping new coverage mandates, but it does extend and normalize care delivery models that require stronger utilization management, vendor oversight, and clinical review infrastructure.
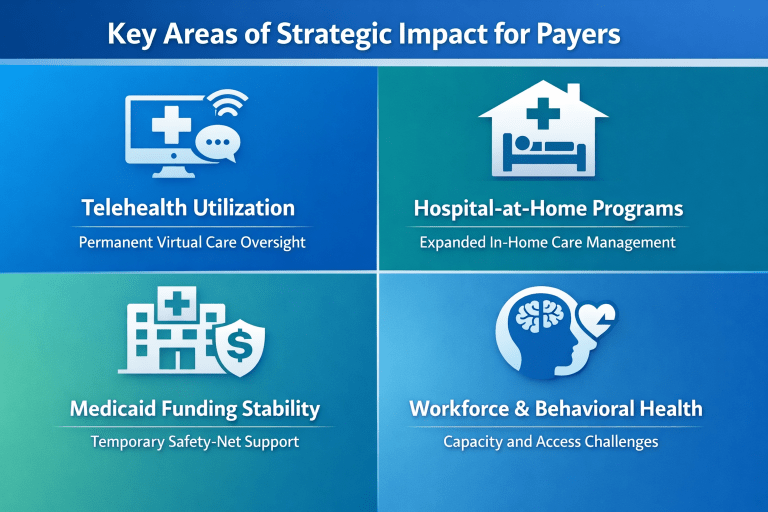
For payers, the Act concentrates its impact across four strategic areas that influence utilization, oversight, and financial stability.
(click each section below to expand)
By extending Medicare telehealth flexibilities through December 31, 2027, the Act effectively removes near-term uncertainty around virtual care reimbursement. Home-based telehealth, audio-only services, and the continued participation of RHCs and FQHCs as distant-site providers are no longer transitional accommodations.
For payers, this solidifies telehealth as a permanent utilization channel rather than an exception. The new requirement for unique billing codes when providers contract with third-party telehealth platforms increases claims complexity and heightens the need for contract-aligned review, billing validation, and fraud, waste, and abuse monitoring.
The five-year extension of the Acute Hospital Care at Home waiver through 2030 signals continued federal support for inpatient-level care delivered outside traditional hospital settings. While these models offer cost and capacity advantages, they also introduce variability in clinical protocols, staffing, and documentation.
Payers should view this extension as a signal to strengthen medical necessity review, peer review standards, and outcome monitoring for hospital-at-home programs, particularly as participation expands beyond early adopters.
Executive Summary
The Consolidated Appropriations Act, 2026 is best understood as a stabilization measure rather than a transformation bill. It extends existing flexibilities and funding streams that normalize alternative care models and delay major funding disruptions.
For payer organizations, the primary implication is not new compliance obligations, but sustained pressure to govern increasingly complex care delivery environments with disciplined utilization management and independent review frameworks.
As care delivery models continue to evolve, BHM Healthcare Solutions supports payer organizations with independent clinical review, utilization management expertise, and quality oversight to help coverage decisions remain consistent, defensible, and aligned with evolving regulatory expectations.
Previous Alerts
Sources
- The White House
Congressional Bill H.R. 7148 Signed Into Law. February 3, 2026. - U.S. House Committee on Appropriations
House Passes H.R. 7148 and H.R. 7147 Completing FY 2026 Appropriations. January 22, 2026. - Congressional Budget Office (CBO)
H.R. 7148, Consolidated Appropriations Act, 2026: Cost Estimate. - Centers for Medicare & Medicaid Services (CMS)
Medicare Telehealth Services and Flexibilities. - American Hospital Association (AHA)
Appropriations Package Extends Key Health Care Provisions. January 2026. - Congress.gov
H.R.7148 – Consolidated Appropriations Act, 2026
- The White House
FAQs
- How does the Consolidated Appropriations Act, 2026 affect healthcare payers?
The Act extends telehealth and hospital-at-home programs, increasing payer responsibility for utilization management, clinical oversight, and coverage consistency across nontraditional care settings. - What changes does the Act make to Medicare telehealth?
It extends Medicare telehealth flexibilities through December 31, 2027, including home-based services, audio-only visits, and continued use of rural and community providers as distant-site clinicians. - What is the impact of delaying Medicaid DSH payment reductions?
The delay preserves Medicaid funding stability for safety-net hospitals through 2028 but does not eliminate longer-term financial pressure on state Medicaid programs. - Why is independent clinical review important under this legislation?
Expanded care models increase variability in care delivery, making independent clinical review essential for defensible coverage decisions, regulatory alignment, and quality oversight.
Each week, we email a summary along with links to our newest articles and resources. From time to time, we also send urgent news updates with important, time-sensitive details.
Please fill out the form to subscribe.
Note: We do not share our email subscriber information and you can unsubscribe at any time.
|
|
Thank you for Signing Up |

Partner with BHM Healthcare Solutions
BHM Healthcare Solutions offers expert consulting services to guide your organization through price transparency & other regulatory complexities for optimal operational efficiency. We leverage over 20 years of experience helping payers navigate evolving prior authorization requirements with efficiency, accuracy, and transparency.
Our proven processes reduce administrative errors, accelerate turnaround times, and strengthen provider relationships, while advanced reporting and analytics support compliance readiness and audit preparation. From operational improvements to strategic positioning, we partner with organizations to turn regulatory change into an opportunity for clinical and business excellence.
