ACA Acronyms | FFOF | Everything Has an Abbrev.

What do the ACA, ACO, FFS, DHS, and QHP all have in common? They are healthcare acronyms and most are related to the Affordable Care Act.
The healthcare industry is not unlike any other industry or almost any aspect of our lives these days, especially with the advent of texting. There is always a shorter way to say something i.e. “BFF” – best friends forever or one of my favorites “*$” – Starbucks. By the way, the title “FFOF” is Fun Facts on Friday.
The ACA, which is part of the “PPACA” – Patient Protection and Affordable Care Act of 2010, is regulated by “HHS” – the division of Health and Human Services, the “DOL” – Department of Labor and the “IRS” – Internal Revenue Service. HHS designates many responsibilities to “CMS” – the Centers for Medicare and Medicaid Services.
Show Me the Money | Profitability Through Value-Based Purchasing

Summary: Are you ready for a shift in risk from payer to provider? Will you be ready for value-based purchasing when it becomes required? Are you utilizing other reimbursement models such as bundled payments, Accountable Care Organizations, and Population Health Management?
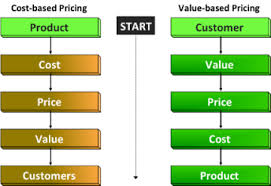
From a provider perspective, healthcare reform is aimed at tightening the purse strings, working more efficiently, reducing waste, and improving quality. The shift of risk has begun which will transform healthcare from a fee-for-service to fee-for-value. When the ultimate transformation ends, is still uncertain. As such, fee-for-service is still being utilized and providers are still generating profits and revenue based on the volume mentality while simultaneously trying to transition to a volume and quantity mentality. Juggling the opposite ends of the spectrum is no easy task.
Shifting Risk: A Pharmacy Perspective on Value-Based Purchasing
Summary: In this article we will discuss Value-Based Purchasing and how it impacts the Pharma industry in particular.
According to an issue brief by Deloitte Center for Health Solutions, Value-based pricing for pharmaceuticals: Implications of the shift from volume to value, a shift in risk is occurring in the pharma industry as a result of healthcare legislation, culminating with the Affordable Care Act (ACA).
ACOs Rapidly Expanding Across States

Accountable Care Organizations (ACOs) are gaining in popularity as a result of the ACA. BHM Healthcare Solutions, a healthcare management consulting firm, has a team of experts dedicated to providing assistance to organizations as they transition from a traditional fee-for-service model to an ACOs assisting in the critical transition to provide quality of care..
Factors Influencing ACO Expansion

Summary: What is contributing to the rapid expansion of ACOs? What programs are currently being piloted? What are the initial results of current ACOs?
What is an ACO?
An ACO is a group of healthcare providers who work together and accept accountability for reducing costs and increasing quality of care.
Preparing for an Accountable Care Organization Conversion

Summary: Accountable Care Organization are becoming more prevalent. Are you in the process of deciding whether or not to become an ACO? Do you have the facts you need to make the right choice?
The ABCs of the Physician Payments Sunshine Act
The Physician Payments Sunshine Act final rule was announced by CMS in February 2013 and requires public disclosure of transfers in value by manufacturers of medical devices and drugs.
Cancer Patients are Seeing the Ripple Effects from the Sequestration
The Patient Protection Affordable Care Act (PPACA) seeks to provide accessible affordable care to more Americans. However, the ripple effects of the sequestration (to Medicare patients undergoing cancer treatments) are in direct contrast to these goals and principles.





