Year End Report
Prior Auth in 2025: Signals for 2026
Why Utilization Management Became the First Accountability Test
Part 2 of 4
In Part 1 of the 2025 in Review series, we outlined how 2025 unfolded differently than most healthcare leaders anticipated. Familiar pressures did not simply intensify. They converged. Regulatory oversight expanded, utilization rose with higher acuity, artificial intelligence entered core workflows, and transparency expectations exposed inconsistencies that once stayed internal.
Prior authorization was the first place those forces collided.
What many organizations expected to remain an administrative pressure point instead became a visible indicator of operational discipline, clinical consistency, and organizational credibility. In 2025, prior authorization moved from a background function to a central lens through which access, affordability, and accountability are now assessed.
Part 2 of the series examines how prior authorization actually evolved in 2025, why it now functions as a bellwether for broader utilization management maturity, and what the signals emerging from this shift suggest for 2026.
This article is Part 2 of a four-part series designed to help payer and UM executives re-calibrate.

Expectations for Prior Authorization in 2025
Heading into 2025, industry analysts and advisory firms largely aligned on a familiar outlook for prior authorization:
- Continued criticism of administrative burden and provider workload
- Incremental regulatory action focused on timeliness and transparency
- Stable denial and appeal volumes within existing frameworks
- Gradual adoption of AI to support clinical review efficiency
- Ongoing network adequacy and access challenges, particularly in Medicaid
The prevailing assumption was that prior authorization would remain highly visible but largely evolutionary. Most organizations anticipated the need for process refinement rather than structural change.
As we mentioned in Part 1, that assumption proved incomplete.

While forecasts correctly identified the direction of change, they underestimated its speed and cumulative impact. Several dynamics accelerated at the same time.
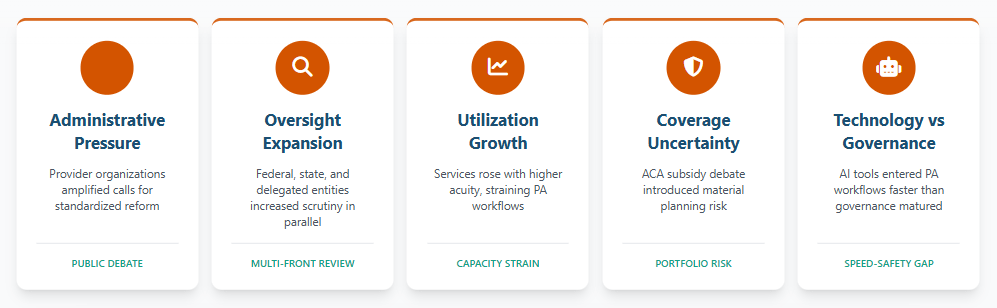
Administrative Pressure Intensified
Provider organizations, including national hospital and specialty groups, amplified calls for standardized prior authorization reform. Prior authorization moved to the center of policy discussions, media scrutiny, and public debate, elevating its visibility and political sensitivity.
Oversight Expanded Across Multiple Fronts
Federal, state, and delegated oversight entities increased scrutiny in parallel. Evaluation extended beyond turnaround times to include decision rationale, documentation quality, and appeal handling. Many organizations found themselves responding to multiple oversight bodies operating simultaneously.
Utilization Rose With Higher Acuity
Behavioral health services, maternal health, complex imaging, and outpatient procedures increased, often within populations facing greater clinical and social complexity. This placed sustained strain on prior authorization workflows and review capacity.
Coverage Uncertainty Grew
Debate surrounding the future of enhanced ACA subsidies introduced material planning risk, particularly for individual and Medicaid lines of business. Shifting membership profiles increased sensitivity to variability in medical necessity determinations.
Technology Adoption Outpaced Governance
AI-enabled tools entered prior authorization workflows faster than organizations could standardize clinical rationale, documentation expectations, and oversight models. What began as efficiency support increasingly influenced decision-making consistency and defensibility.
Taken together, these forces did not simply increase volume or speed requirements. They raised expectations for consistency, reproducibility, and clinical coherence under sustained scrutiny.
The Year Prior Authorization Went Public
Prior authorization sits at the intersection of utilization, clinical judgment, compliance, and member experience. In 2025, that positioning made it the first function where broader system stress became visible.
As utilization increased and oversight expanded, variability that might once have been tolerated became harder to defend. Documentation quality, appeal outcomes, and decision logic increasingly served as proxies for organizational maturity.
In effect, prior authorization shifted from a utilization control mechanism to a public accountability function.
Why Prior Auth = The Bellwether
Top Signals for 2026
ACA Subsidies and Membership Volatility
The potential expiration of enhanced ACA subsidies represents the most significant external variable shaping prior authorization strategy.
If subsidies lapse without a viable alternative, organizations may face:
- Reduced premium inflows
- Membership shifts across commercial, Medicaid, and uninsured populations
- Higher acuity concentrations within remaining covered lives
- Increased pressure to maintain network adequacy
- Greater scrutiny of access, denials, redeterminations, and maternal health outcomes
Prior authorization programs are calibrated to specific risk profiles. As those profiles change, tolerance for variability in medical necessity decisions narrows, and expectations for precision increase.
Accelerating Oversight and Decision Scrutiny
Regulatory momentum in 2025 made clear that prior authorization reform is no longer conceptual.
Oversight is increasingly focused on:
- How decisions are made
- How clinical rationale is documented
- How consistently decisions can be reproduced
- How appeals outcomes align with stated policies
This evolution reframes prior authorization as a visible measure of organizational discipline rather than a back-office process.
The WISeR Model as a Signal, Not a Pilot
One of the most consequential developments heading into 2026 is CMS’s WISeR model.
Beginning in January, WISeR will operate in six states with six participating vendors, introducing a technology-forward framework for evaluating:
- Prior authorization processes
- Documentation quality and structure
- Program transparency
- Decision consistency
While its initial scope is limited, WISeR is best understood as a directional signal. It introduces the concept of continuous, data-driven oversight supported by AI-generated insights.
For payer and UM leaders, the strategic questions extend beyond participation:
- How will CMS interpret and act on WISeR findings?
- Will early results influence broader enforcement expectations?
- How quickly might similar evaluation models scale nationally?
WISeR suggests a future in which prior authorization programs are assessed against standardized benchmarks, with increasing reliance on structured data to validate clinical decision-making.
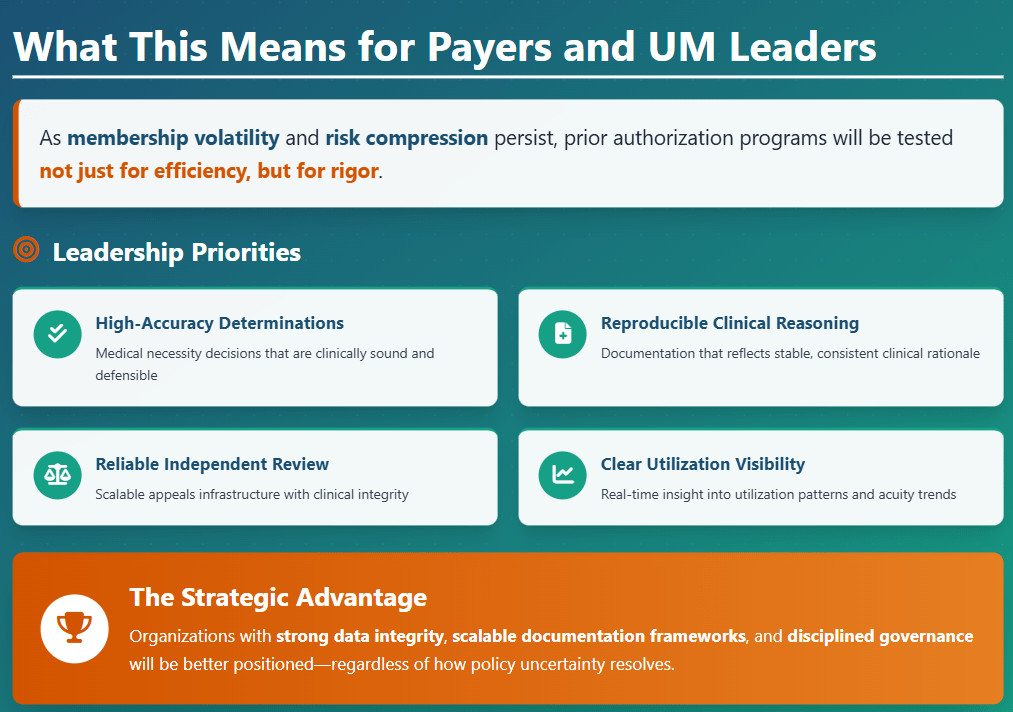
What Happens Next
The trajectory for prior authorization is becoming clearer. Oversight is expanding. Transparency expectations are rising. AI-enabled evaluation models are beginning to influence how utilization management programs are judged.
For executives, the opportunity is to treat these developments not simply as compliance obligations, but as early indicators of where utilization management is headed. Investments made now in documentation quality, clinical alignment, and review infrastructure will shape how confidently organizations navigate 2026.
Part 3 in this series examines how artificial intelligence is being leveraged across utilization management and related operations, and why governance, not adoption, is emerging as the defining challenge for healthcare leaders.
Frequently Asked Questions (FAQs)
Why did prior authorization become a focal point in healthcare during 2025?
In 2025, prior authorization became a focal point because rising utilization, expanded regulatory oversight, and increased transparency expectations converged at the same time. As scrutiny shifted beyond turnaround times to decision rationale and appeal outcomes, prior authorization emerged as a visible measure of organizational discipline and clinical consistency.
What does prior authorization reform in 2025 signal for 2026?
The changes seen in 2025 suggest that prior authorization programs will be evaluated in 2026 not just for efficiency, but for rigor. Expectations are rising around reproducible medical necessity decisions, documentation quality, and the ability to demonstrate consistency across populations and oversight bodies.
How does AI affect prior authorization oversight and accountability?
AI increasingly supports prior authorization workflows by assisting with documentation, utilization analysis, and operational efficiency. However, as AI outputs influence decision-making, organizations face greater expectations to govern how those tools are used, explain their role in determinations, and align them with clinical oversight and regulatory standards.
Why Choose BHM?
We proudly stand behind our reputation in the industry as experts in utilization management.
Our proven process has served our clients well for over 20 years and our unwavering focus on serving clients with excellence has set us apart.
Here are a few ways we demonstrate that commitment.

Trust
Reliable Partner
We’ve built our reputation on integrity, transparency, and delivering dependable services that organizations trust to support critical decisions in cost effective care.
Expertise
Industry Knowledge
Our team of seasoned professionals and clinical experts provide unparalleled insights and guidance tailored to meet the complex needs of healthcare payers and providers.

Innovation
Driving Progress
We combine advanced technologies and forward-thinking strategies to deliver efficient, scalable solutions that enhance outcomes and streamline processes.

Outcomes
Measurable Impact
Our systems are designed to employ data-driven insights to help organizations improve quality, reduce costs, and meet compliance standards for lasting success.
Partner with BHM Healthcare Solutions
With over 20 years in the industry, BHM Healthcare Solutions is committed to providing consulting and review services that help streamline clinical, financial, and operational processes to improve care delivery and organizational performance.
We bring the expertise, strategy, and capacity that healthcare organizations need to navigate today’s challenges – so they can focus on helping others.
Are you ready to make the shift to a more effective process?

