Year End Report
What 2025 Signals for 2026
A Review of the Forces Reshaping Healthcare Leadership
Part 1 of 4
Healthcare leaders entered 2025 anticipating pressure, but not disruption. Analysts pointed to familiar headwinds: regulatory scrutiny, margin compression, utilization growth, and continued digital expansion. The prevailing assumption was that the year would be difficult but manageable, requiring refinement rather than reinvention.
Twelve months later, that assumption no longer holds.
The pace and convergence of change in 2025 created a level of operational volatility that many payer and utilization management leaders did not plan for. Regulatory oversight accelerated, prior authorization reform intensified, artificial intelligence moved rapidly into core workflows, and transparency expectations exposed inconsistencies across clinical, operational, and financial domains.
This article is Part 1 of a four-part series designed to help payer and UM executives re-calibrate.

What Analysts Expected for 2025
Entering 2025, major advisory firms largely aligned around a consistent outlook for healthcare organizations:
- Membership instability driven by Medicaid re-determinations
- Modest individual market growth supported by enhanced ACA subsidies
- Slower cost growth due to economic pressure
- Increased regulatory scrutiny of prior authorization and appeals
- Persistent network adequacy challenges
- Continued expansion of value-based payment models
The dominant interpretation was that 2025 would require discipline and adaptability, but that it would largely extend existing trajectories rather than fundamentally disrupt them.
That framing proved incomplete.

Most forecasts correctly identified the direction of change, but underestimated its velocity and interaction effects. Several forces accelerated simultaneously:
Membership Volatility Intensified
Re-determinations moved faster than anticipated. Commercial enrollment fluctuated, and state-level policy decisions altered risk profiles across payer portfolios. Planning assumptions tied to stable population segments became less reliable.
Utilization Increased With Higher Acuity
Behavioral health services, maternal health, complex imaging, and outpatient procedures rose, often concentrated among populations with greater clinical and social complexity. This placed additional strain on utilization management programs and appeals infrastructure.
Regulatory Oversight Expanded
Federal and state agencies advanced new documentation, reporting, transparency, and compliance expectations, often in parallel. Oversight became more granular and more frequent, increasing scrutiny of how decisions are made and justified.
Coverage Uncertainty Grew
Ongoing debate surrounding the future of enhanced ACA subsidies introduced material planning risk, particularly for Medicaid and individual market strategies.
AI Adoption Outpaced Governance
Clinical and administrative AI tools entered workflows faster than many organizations could formalize oversight, validation, and accountability frameworks, introducing operational inconsistency and governance exposure.
These developments did not occur in isolation. Together, they reshaped how utilization management programs, appeals workflows, compliance teams, and clinical leadership functions are evaluated.
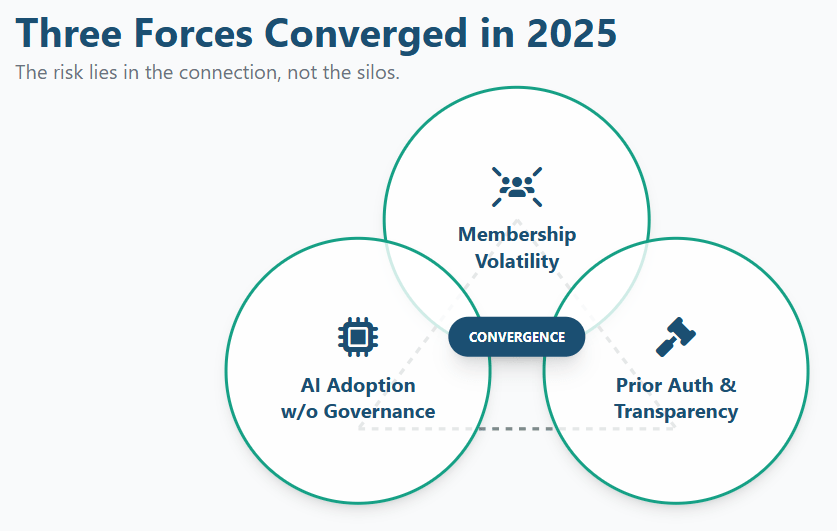
Why These Forces Now Intersect
What made 2025 materially different was not the presence of these pressures, but their convergence.
- Prior authorization reform increased demands for speed, consistency, and defensible clinical rationale.
- AI tools were increasingly used to support documentation, utilization review, and operational efficiency, often without standardized governance.
- At the same time, transparency requirements made internal inconsistencies visible to regulators, purchasers, and the public.
As a result, decisions that once stayed inside operational silos are now subject to external interpretation. Documentation quality, decision logic, and data alignment have become indicators of organizational discipline, not just compliance.
This convergence reframes familiar challenges into a single question:
Can healthcare organizations explain and defend how decisions are made across clinical, operational, and financial domains?
Three Forces That Reshaped 2025
Prior Authorization Reform
Prior authorization moved from a background administrative concern to a central accountability function. Policymakers, providers, and oversight bodies increased scrutiny of decision timeliness, rationale, and appeal handling. At the same time, utilization rose in higher-acuity populations, placing additional pressure on PA workflows and documentation consistency.
This shift elevated prior authorization as a visible reflection of operational maturity rather than a purely administrative process.
Part 2 of this series examines how prior authorization reform, transparency expectations, and appeals pressure converged in 2025 and why this function now serves as a bellwether for 2026 readiness.
AI Adoption and Governance
Artificial intelligence moved rapidly from pilot programs to embedded operational tools. AI-enabled solutions increasingly influence documentation, utilization patterns, and administrative workflows. However, governance frameworks often lagged deployment.
As AI outputs became more central to decision-making, questions of accountability, explainability, and oversight moved from technical teams to executive leadership.
Part 3 explores how AI adoption in 2025 introduced new operational and reputational risks, and why governance maturity is emerging as the defining challenge for 2026.
Transparency, Efficiency, and Accountability
Transparency requirements expanded beyond price posting into broader evaluations of access, efficiency, and outcomes. Regulators and purchasers increasingly assessed whether reported data told a coherent story across domains.
Efficiency became externally visible. Accountability shifted from process adherence to outcome explanation. Misalignment between financial, clinical, and operational narratives became harder to obscure.
Part 4 examines how transparency, efficiency, and accountability now function as a single system and what this means for sustainable utilization management models.
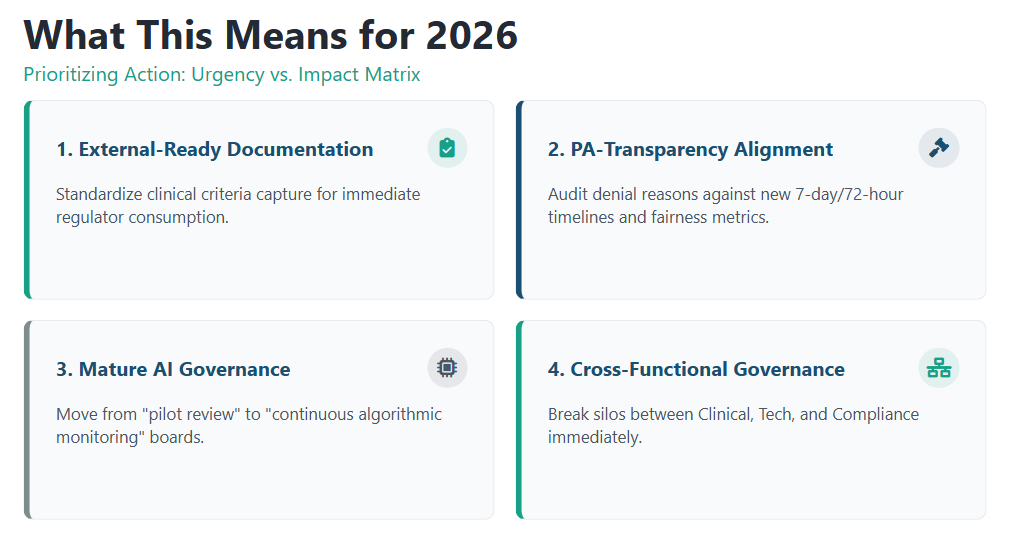
What Happens Next
The forces shaping 2026 are already evident: expanding oversight, shifting coverage patterns, rising utilization, AI-enabled monitoring, and increased transparency.
Organizations best positioned for the year ahead are using lessons from 2025 to:
- Strengthen documentation and clinical rationale across UM workflows
- Align prior authorization policies with transparency expectations
- Clarify how AI-supported findings are interpreted and governed
- Improve collaboration across compliance, medical leadership, operations, and UM teams
That progression sets the foundation for the remainder of this series.
Frequently Asked Questions (FAQs)
What were the biggest changes in healthcare during 2025?
In 2025, healthcare experienced accelerated regulatory oversight, increased utilization with higher acuity, rapid expansion of prior authorization reform, broader adoption of AI in operational workflows, and heightened transparency expectations. While many of these trends were anticipated, their speed and combined impact created more operational volatility than most organizations planned for.
Why did healthcare leaders underestimate the impact of 2025 changes?
Most forecasts correctly identified the direction of change but underestimated how quickly multiple forces would converge. Prior authorization reform, AI adoption, and transparency requirements advanced simultaneously, exposing governance gaps and operational inconsistencies that were not apparent when these pressures were managed independently.
How did prior authorization become more important in 2025?
Prior authorization shifted from a background administrative process to a visible accountability function. Expanded oversight, higher utilization in complex populations, and greater scrutiny of documentation and appeals elevated prior authorization as a key indicator of organizational discipline and clinical consistency.
What role did artificial intelligence play in healthcare operations in 2025?
AI moved from limited pilots to embedded use across clinical and administrative workflows in 2025. While these tools improved efficiency, governance frameworks often lagged deployment, raising questions around accountability, explainability, and executive oversight as AI outputs increasingly influenced operational decisions.
Why are transparency and accountability now central leadership issues?
Transparency requirements in 2025 extended beyond reporting compliance to evaluating whether organizations could present consistent, defensible narratives across cost, access, quality, and utilization. Efficiency and accountability became externally visible, making data alignment and documentation quality leadership responsibilities rather than technical tasks.
More in this series...
What Transparency in 2025 Signals for 2026
A review of how transparency evolved in 2025, why it…
What AI Adoption in 2025 Signals for 2026
A review of how AI adoption accelerated in 2025, why…
What Prior Authorization in 2025 Signals for 2026
A review of how prior authorization evolved in 2025, why…
Why Choose BHM?
We proudly stand behind our reputation in the industry as experts in utilization management.
Our proven process has served our clients well for over 20 years and our unwavering focus on serving clients with excellence has set us apart.
Here are a few ways we demonstrate that commitment.

Trust
Reliable Partner
We’ve built our reputation on integrity, transparency, and delivering dependable services that organizations trust to support critical decisions in cost effective care.
Expertise
Industry Knowledge
Our team of seasoned professionals and clinical experts provide unparalleled insights and guidance tailored to meet the complex needs of healthcare payers and providers.

Innovation
Driving Progress
We combine advanced technologies and forward-thinking strategies to deliver efficient, scalable solutions that enhance outcomes and streamline processes.

Outcomes
Measurable Impact
Our systems are designed to employ data-driven insights to help organizations improve quality, reduce costs, and meet compliance standards for lasting success.
Partner with BHM Healthcare Solutions
With over 20 years in the industry, BHM Healthcare Solutions is committed to providing consulting and review services that help streamline clinical, financial, and operational processes to improve care delivery and organizational performance.
We bring the expertise, strategy, and capacity that healthcare organizations need to navigate today’s challenges – so they can focus on helping others.
Are you ready to make the shift to a more effective process?