Year End Report
Transparency in 2025
Why Credibility Became the Ultimate Accountability Test
Part 4 of 4
In Part 1 of this series, we outlined how familiar pressures in healthcare converged in unexpected ways during 2025. In Part 2, we examined how prior authorization became the first visible accountability test. In Part 3, we explored how AI adoption introduced new governance and decision-ownership challenges.
Transparency is where all of those forces became externally visible.
In 2025, transparency, efficiency, and accountability stopped functioning as separate initiatives. What had long been treated as a compliance-driven reporting exercise evolved into a defining test of organizational credibility. Pricing disclosures, quality reporting, utilization oversight, and operational performance are now evaluated together, shaping how payers, regulators, purchasers, and patients assess trustworthiness and value.
For healthcare executives, the implication is clear: transparency has moved from disclosure to discipline.
This article is Part 4 of a four-part series designed to help payer and UM executives re-calibrate.

What Analysts Expected for 2025
- And Why That View Fell Short
Heading into 2025, analysts largely anticipated steady but manageable progress:
- Continued expansion of price transparency and reporting mandates
- Incremental enforcement tied to existing rules
- Gradual efficiency gains through automation
- Persistent challenges aligning cost, quality, and access metrics
- Limited behavioral change driven by transparency data alone
The dominant assumption was that transparency would remain reporting-oriented: important, but peripheral to core operating decisions.
What this framing underestimated was convergence. Pricing files, quality scores, utilization metrics, and access indicators increasingly intersected, making inconsistencies harder to obscure and easier to compare.
Fragmented data strategies that once sufficed began to create visible contradictions:
- Between posted prices and patient bills
- Between access commitments and network performance
- Between quality claims and utilization outcomes

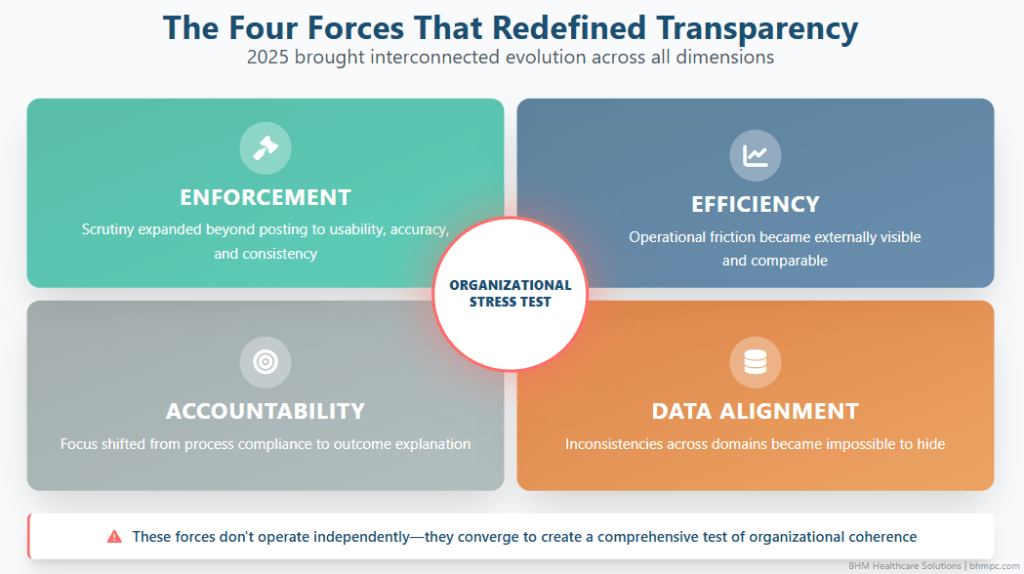
How Transparency and Accountability Actually Evolved in 2025
In practice, 2025 brought faster, more interconnected change that raised expectations across the system.
Enforcement Became More Credible
Regulators increased scrutiny not just of whether data was posted, but whether it was usable, accurate, and internally consistent. Transparency failures began carrying reputational and financial consequences, not just technical remediation.
Efficiency Became Externally Visible
Delays in care, billing complexity, and administrative friction became measurable and comparable across organizations. Inefficiency shifted from an internal cost issue to a visible signal of stewardship.
Accountability Shifted Toward Outcomes
Oversight expanded from process compliance to outcome explanation. Organizations were increasingly expected to explain why access, affordability, and equity outcomes looked the way they did, not simply confirm that policies were followed.
Data Alignment Gaps Were Exposed
Differences between finance, operations, clinical quality, and compliance narratives became harder to reconcile as datasets converged. Inconsistent internal metrics began undermining external credibility.
Together, these forces elevated transparency from a reporting requirement to an organizational stress test.
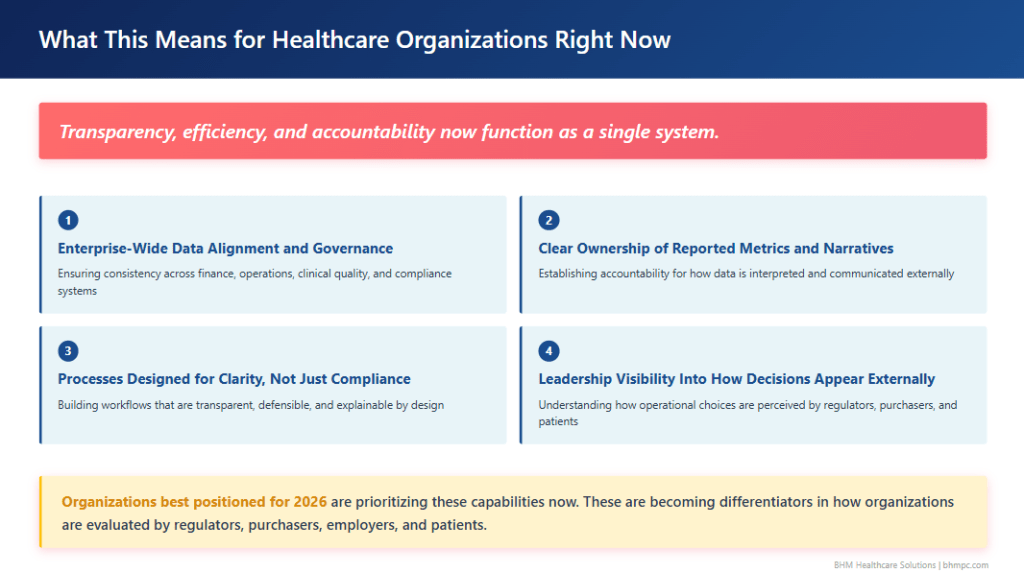
One Unified System
Transparency, efficiency, and accountability now function as a single system. Organizations best positioned for 2026 are prioritizing:
- Enterprise-wide data alignment and governance
- Clear ownership of reported metrics and narratives
- Processes designed for clarity, not just compliance
- Leadership visibility into how operational decisions appear externally
These capabilities are becoming differentiators in terms of how organizations are evaluated by regulators, purchasers, employers, and patients.
Where Transparency Becomes Strategic
Top Signals for 2026
Transparency Will Be Used to Judge Organizational Coherence
In 2026, transparency will increasingly be used to assess whether an organization operates as a coordinated system.
Expect scrutiny of:
- Alignment between posted prices, contracted rates, and patient responsibility
- Consistency between access commitments and actual utilization patterns
- Coherence between quality measures and resource use
Organizations unable to reconcile these domains will face questions that extend beyond compliance into leadership credibility.
Efficiency Will Be Treated as an Accountability Measure
Efficiency is no longer viewed solely as cost control. It is increasingly evaluated as a marker of responsible care delivery.
Indicators drawing scrutiny include:
- Administrative complexity that delays care or payment
- Redundant or opaque processes that increase patient burden
- Utilization variation unexplained by clinical need
Operational inefficiency now carries reputational risk. Leaders will be expected to demonstrate simplification, not just savings.
Accountability Will Extend Beyond Individual Metrics
Oversight is moving away from isolated measures toward pattern recognition across time. This includes:
- Longitudinal tracking of access and affordability
- Cross-measure evaluation of cost and quality tradeoffs
- Expanded comparative benchmarking
Short-term optimization of individual metrics may backfire if it creates visible downstream effects. Strategic consistency will matter more than isolated performance wins.
Collective Signals
Taken together, the lessons of 2025 are not about new rules or isolated reforms. They are about visibility:
- Prior authorization revealed how decisions are made
- AI governance exposed who owns those decisions
- Transparency determines how those decisions are judged
In 2026, healthcare organizations will not be assessed solely on outcomes, innovation, or compliance. They will be assessed on whether they can explain their decisions clearly, consistently, and credibly under scrutiny.
Leaders who treat documentation, governance, and transparency as strategic infrastructure will be better positioned to navigate the year ahead. Those who do not may find that the true cost of accountability emerges not in regulation, but in trust.
This four-part series was designed to help payer and utilization management leaders recalibrate after a year that unfolded faster and more forcefully than expected. The signals from 2025 are already shaping 2026. The organizations that respond most effectively will be those that recognize these developments not as isolated pressures, but as a connected system redefining healthcare leadership.
Frequently Asked Questions (FAQs)
Why did transparency become a leadership issue in healthcare during 2025?
Transparency became a leadership issue in 2025 because reporting requirements converged across pricing, quality, utilization, and access. Regulators and purchasers increasingly evaluated whether organizations could present consistent, defensible narratives across these domains, shifting transparency from a compliance task to a test of organizational credibility.
How are efficiency and accountability connected to transparency in healthcare?
In 2025, efficiency and accountability became externally visible through transparency data. Delays in care, administrative complexity, and unexplained utilization variation increasingly signaled poor stewardship. As a result, efficiency is now evaluated not only as a cost concern, but as an accountability measure tied to trust and performance.
What do transparency trends from 2025 signal for healthcare organizations in 2026?
The transparency trends of 2025 signal that in 2026, organizations will be judged less on individual metrics and more on coherence across systems. Expectations are rising around data alignment, outcome explanation, and the ability to demonstrate how policies, incentives, and decisions interact over time.
Why Choose BHM?
We proudly stand behind our reputation in the industry as experts in utilization management.
Our proven process has served our clients well for over 20 years and our unwavering focus on serving clients with excellence has set us apart.
Here are a few ways we demonstrate that commitment.

Trust
Reliable Partner
We’ve built our reputation on integrity, transparency, and delivering dependable services that organizations trust to support critical decisions in cost effective care.
Expertise
Industry Knowledge
Our team of seasoned professionals and clinical experts provide unparalleled insights and guidance tailored to meet the complex needs of healthcare payers and providers.

Innovation
Driving Progress
We combine advanced technologies and forward-thinking strategies to deliver efficient, scalable solutions that enhance outcomes and streamline processes.

Outcomes
Measurable Impact
Our systems are designed to employ data-driven insights to help organizations improve quality, reduce costs, and meet compliance standards for lasting success.
Partner with BHM Healthcare Solutions
With over 20 years in the industry, BHM Healthcare Solutions is committed to providing consulting and review services that help streamline clinical, financial, and operational processes to improve care delivery and organizational performance.
We bring the expertise, strategy, and capacity that healthcare organizations need to navigate today’s challenges – so they can focus on helping others.
Are you ready to make the shift to a more effective process?

