Show Me the Money | Profitability Through Value-Based Purchasing
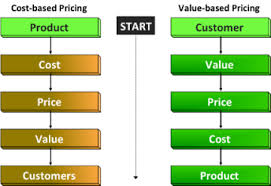
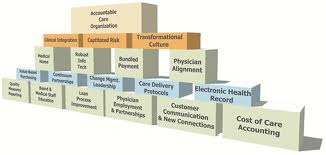
Summary: Are you ready for a shift in risk from payer to provider? Will you be ready for value-based purchasing when it becomes required? Are you utilizing other reimbursement models such as bundled payments, Accountable Care Organizations, and Population Health Management? From a provider perspective, healthcare reform is aimed at tightening the purse strings, working more efficiently, reducing waste, and improving quality. The shift of risk has begun which will transform healthcare from a fee-for-service to fee-for-value. When the ultimate transformation ends, is still uncertain. As such, fee-for-service is still being utilized and providers are still generating profits and revenue based on the volume mentality while simultaneously trying to transition to a volume and quantity mentality. Juggling the opposite ends of the spectrum is no easy task.