Shifting Risk: A Pharmacy Perspective on Value-Based Purchasing
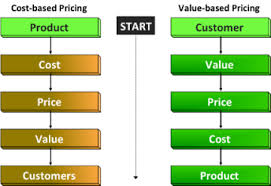
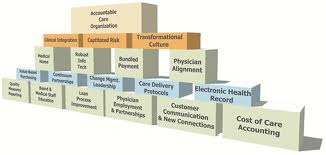
Summary: In this article we will discuss Value-Based Purchasing and how it impacts the Pharma industry in particular. According to an issue brief by Deloitte Center for Health Solutions, Value-based pricing for pharmaceuticals: Implications of the shift from volume to value, a shift in risk is occurring in the pharma industry as a result of healthcare legislation, culminating with the Affordable Care Act (ACA).