|
From navigating complex regulatory landscapes to meeting the high demands of patient satisfaction, the path to optimizing operations is fraught with obstacles. Yet, in the midst of these challenges lies a significant opportunity for strategic improvements that can streamline processes, reduce efforts, and ultimately enhance the overall performance of healthcare payers.
Understanding the Payer Landscape
The payer industry is at a critical juncture, where operational efficiency is not just a goal but a necessity for survival and success. As healthcare providers, patients, and regulatory bodies evolve in their expectations, payers are under increasing pressure to adapt and respond with more agility and precision. Efficiency in operations directly correlates with a payer’s ability to manage costs, improve patient outcomes, and comply with stringent regulations, making it a cornerstone of sustainable growth in the healthcare sector.
Key Areas to Maximize Efficiencies and Minimize Efforts
Data Management and Analytics
In the age of information, leveraging data analytics is paramount for identifying inefficiencies, predicting healthcare trends, and making informed decisions. By adopting advanced data management solutions, payers can gain valuable insights into their operations, member needs, and market dynamics, enabling them to anticipate changes and adapt strategies accordingly.
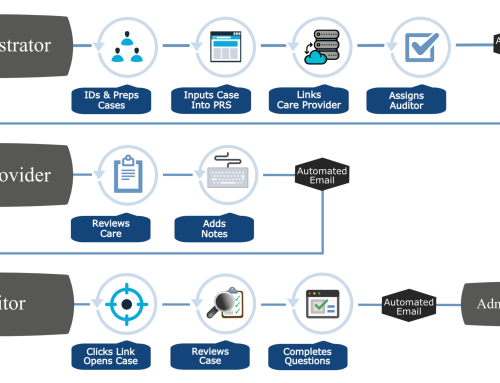
Process Automation
Automating routine tasks not only reduces manual errors but also allows human resources to be allocated to more strategic endeavors. From claims processing to member enrollment, automation can significantly streamline operations, leading to improved efficiency and accuracy.
Provider Network Management
Optimizing provider networks is crucial for ensuring quality care while maintaining cost efficiency. Strategies such as value-based contracting and network design optimization can help payers align with providers who share their commitment to efficiency and patient-centered care.
Member Engagement
Improving member experience is essential for maintaining satisfaction and loyalty. Tailored communication and the use of digital engagement tools can make healthcare more accessible and understandable for members, promoting better health outcomes and more efficient use of healthcare resources.
Step-by-Step Process to Maximize Efficiencies
Assessment and Analysis
The first step involves a thorough review of existing processes to identify inefficiencies and areas for improvement. This foundational analysis sets the stage for targeted interventions that can yield the most significant impact.
Benchmarking
Comparing against industry standards or competitor benchmarks can offer valuable insights into performance gaps and opportunities for enhancement. This step ensures that improvement efforts are aligned with best practices and industry trends.
Strategy Development
Developing a detailed plan is critical for success. This strategy should focus on integrating technology, automating processes, and optimizing workflows to achieve the desired efficiency gains.
Implementation
Changes should be implemented incrementally to minimize disruption to operations. This phased approach allows for adjustments to be made based on real-time feedback and outcomes.
Monitoring and Evaluation
Continuous tracking of the impact of these changes is crucial for understanding their effectiveness and making necessary adjustments. This ongoing evaluation ensures that strategies remain aligned with objectives and adapt to changing conditions.
Leveraging Technology for Efficiency
Emerging technologies such as AI, machine learning, and blockchain hold the potential to revolutionize payer processes. These innovations can enhance decision-making capabilities, streamline administrative tasks, and improve data security, further driving efficiencies in payer operations.
Regulatory Compliance and Risk Management
Improving operational efficiencies is not only about boosting performance but also about enhancing compliance and risk management. Efficient operations can help payers navigate the complex regulatory environment more effectively, reducing the risk of non-compliance and associated penalties.
Embracing Efficiency: The Path Forward for Healthcare Payers
The journey toward maximizing efficiencies and minimizing efforts requires a proactive and systematic approach. By focusing on key areas for improvement, leveraging technology, and continuously evaluating progress, payers can transform their operations and achieve superior performance. Embracing these strategies not only leads to operational excellence but also positions payers to better meet the needs of their members and providers in the evolving healthcare landscape. As such, payers are encouraged to take decisive steps towards adopting these efficiency-maximizing practices, ensuring their operations are not only sustainable but also primed for future success.





Leave A Comment