Observation Units – Bridging the Gap Between Inpatient and Outpatient
What is CMS doing to reduce healthcare costs? CMS has added observation units which are an additional level of care between inpatient and outpatient. What Are Observation Units? In general, observation units are used to bridge the gap between inpatient and outpatient. They are designed for the patient in which the attending physician cannot determine whether a patient should be classified as outpatient (released within 48 hours) or inpatient (expected to stay at least 2 midnights). The observation units enable the physician to have a bit more time to stabilize the patient and based on medical necessity determine the estimated length of stay. They are billed as outpatient and do not count toward an inpatient admission.









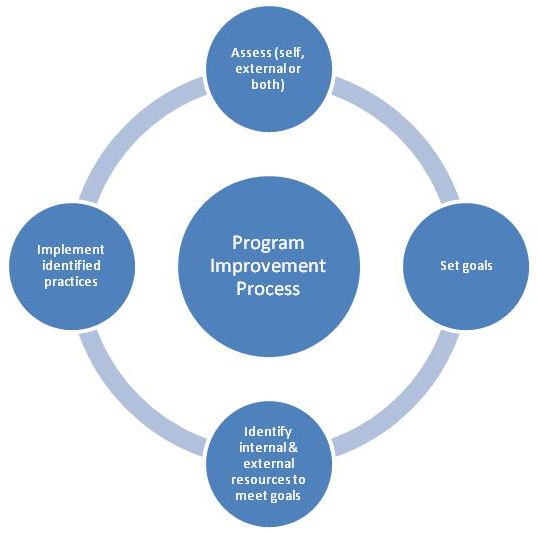
 Why Quality Improvement Programs Are Essential For Today’s Organizations
Why Quality Improvement Programs Are Essential For Today’s Organizations
