Enhancing Collaboration in Medical Necessity Criteria
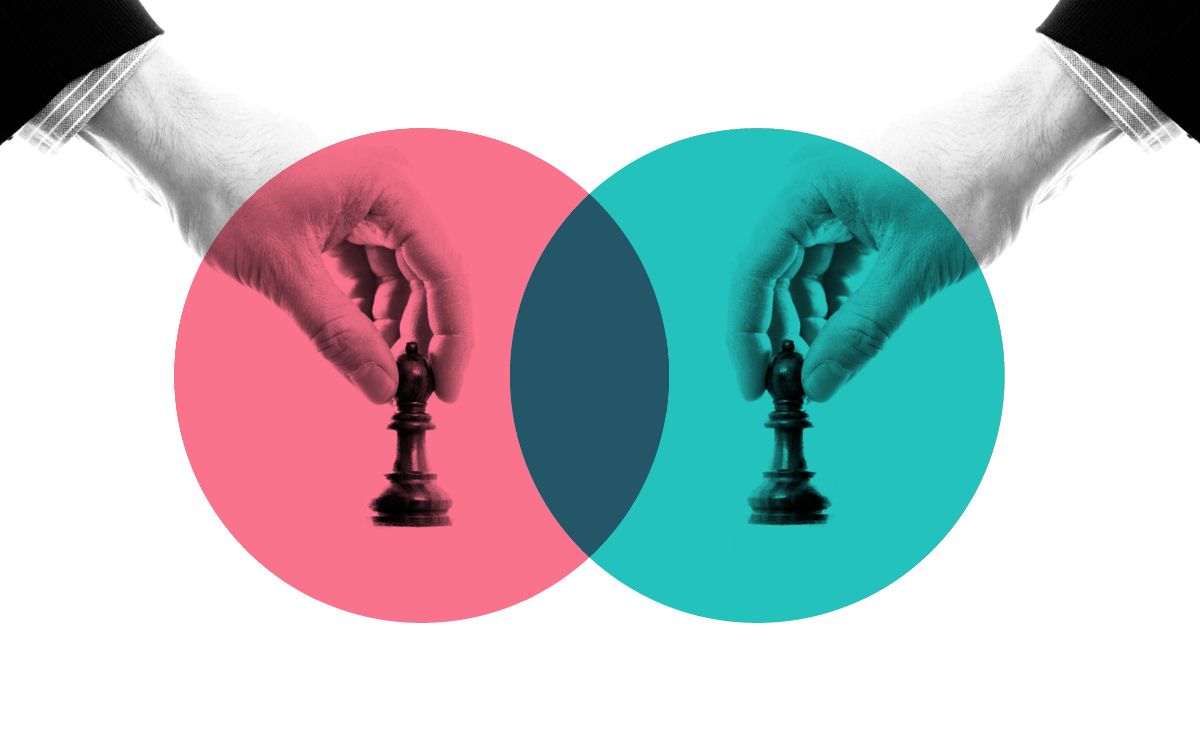
Collaboration between healthcare providers and payers is instrumental in navigating the complexities of medical necessity criteria. By fostering a cooperative environment, both parties can work together to ensure that medical decisions align with the best interests of the patient.