One Year Since CMS Cracked Down on Readmissions | Where Are We Now?
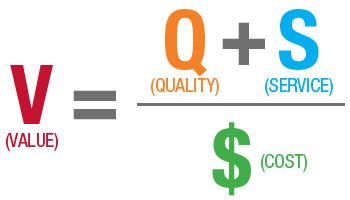
October 1st of last year, CMS cracked down on readmission rates for hospitals nationwide, handing out millions of dollars in penalties. The Affordable Care Act put these measures into place in order to curb the problem of readmissions, which are not only costly, but reflect an overall poor population health in the U.S. - especially for those patients with chronic conditions. For FY ‘14, 2% was withheld from payments per the guidelines for penalties. By 2015, the rate of withholding for penalties is expected to top 3%. In addition to the higher payments, there will also be additional diagnoses included in the readmission criteria list - it began with heart attacks, pneumonia and heart failure and will now expand to include COPD and complications from chronic lung conditions.