9 Criticisms to the Readmission Reduction Program
The Readmission Reduction Program is designed to reduce healthcare spending while improving quality. There are both proponents and opponents of the program. Let’s delve into the improvements that could be made to the current system. So, as most of you are aware, CMS under the direction of HHS created the Hospital Readmission Reduction Program in order to reduce healthcare spending while improving the quality of care. The program is being phased in beginning with a 3 year baseline period in which hospitals were required to report all readmissions (within 30 days). CMS assessed and analyzed all of the available readmission data to determine how penalties should be assessed, for which conditions, and excluding certain circumstances. Beginning in October 2012, penalties were assessed to over 2,200 hospitals, equating to about $280 million. The phase in included an increase in penalties from 2013 to 2015 from 1% to 3%, where it is currently capped. Initially, there were 3 conditions included: Acute Myocardial Infarction, Heart Failure, and Pneumonia. For 2015, CMS is proposing 2 additional conditions: Chronic Obstructive Pulmonary Disease and Elective Hip and Knee Replacements.


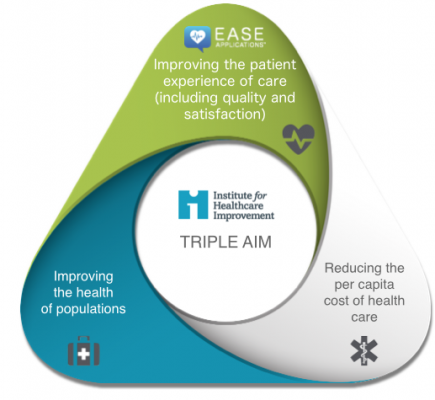


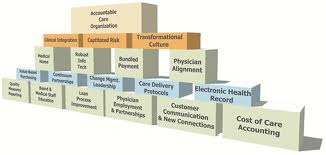


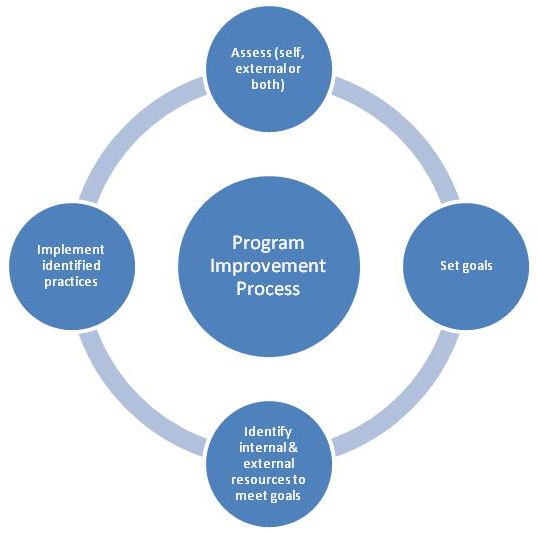
 Why Quality Improvement Programs Are Essential For Today’s Organizations
Why Quality Improvement Programs Are Essential For Today’s Organizations


