The Guiding Light: The Importance of Physician Advisors
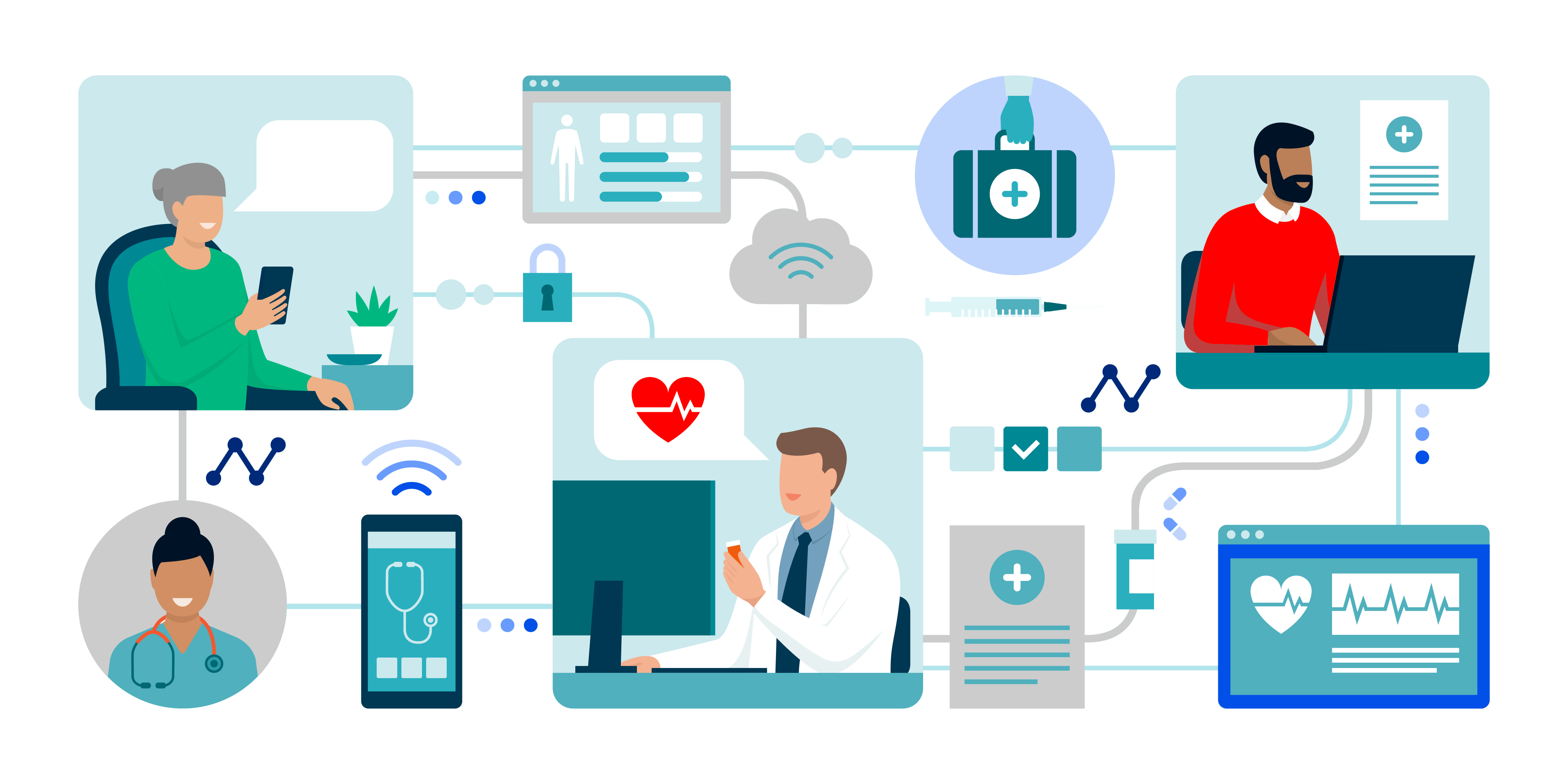
The vast amount of medical information available, combined with the intricacies of various treatment options, can leave patients and their families feeling overwhelmed and uncertain about the best course of action. This is where physician advisors step in to provide invaluable assistance.