Health Insurance Plan Ratings for 2017: NCQA Releases Top 10 List
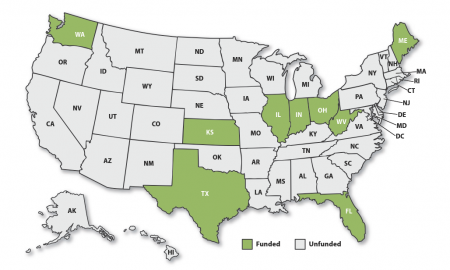
NCQA’s Health Insurance Plan Ratings 2017–2018 compare the quality and services of more than 1,000 health plans in the United States and provide consumers with a practical and meaningful guide to understanding their health care options and choosing the best health plans for themselves and their families. National Committee for Quality Assurance (NCQA) is releasing its 2017 Health Insurance Plan Ratings. These ratings provide consumers with a more accurate picture of how health insurance plans perform in the key quality areas of consumer satisfaction, prevention and treatment.